This policy is available in alternative formats on request. Please contact the Corporate Governance Office on 01204 498400 with your request.
Version | Date of change | Date of release | Changed by | Reason for change |
|---|---|---|---|---|
| 0.1 | ||||
| 0.2 | April 2022 | May 2022 | Kate Shethwood | Update national context, progress in Year 1 and addition of year 2 milestones |
| 0.3 | October 2023 | October 2023 | Steve Bell / Claudia Soiland-Reyes | Scheduled review. Minor changes to Sponsor. |
On this page
1. Introduction
NWAS has a vision to deliver the right care at the right time in the right place, every time. To achieve this, we need to work with communities and partner agencies to deliver preventative initiatives to improve the health of the North West (NW) population and ensure our resources are used in the most effective way.
This document sets out the strategic ambition to embed public health approaches and prevention in NWAS. Public health aims to improve the physical and mental health outcomes and wellbeing of people within a population by focussing on prevention and reducing health inequalities.
This NWAS Public Health Plan was published in April 2021 and updated in 2022. Public Health leadership embedded in NWAS has begun to highlight existing work and identify opportunities to share and develop this, co-ordinating across the Trust and linking to wider sources of information and support.
1.1. Our population
The North West has a population of just over 7.3 million people and covers a total of 5,400 square miles. The urban centres in the region are centred around Manchester and Liverpool which have high population densities (>4000 people per km2). There are also rural areas like Cumbria and Cheshire East which are much less densely populated. 18.7% of the North West population is over 65, with higher proportions of older people in rural areas.
At the 2011 census, the proportion of white people in the region reduced from 94.4% to 90.2%. Within that, 87.1% of the region’s residents were classed as White British, which is higher than the England average of 79.8%. In 2011, 1.2% of people in NW (83,442) were estimated to not speak English well or at all. The distribution of Black and Minority Ethnic populations across the North West is not even and the majority are focused on the Greater Manchester area.
By 2040, the population of the region is projected to grow to 7.85 million people, an increase of 7.5% from 2018. The rate of growth is highest in older age groups; the population aged 90 and over is predicted to double in the next 20 years. This has important implications for NWAS demand as older age groups are heavier users of our service.
1.2. Deprivation
The Index of Multiple Deprivation 2019 is a relative measure of deprivation measured across seven distinct domains: income, health and disability, employment, education, skills and training, barriers to housing and services, crime, and living environment. Area level deprivation strongly links to health inequalities through increased risk of disease and different experiences of care, including the risk of hospitalisation and deaths from COVID-19. Public Health Plan Page: 6 Author: Christine Camacho Version: 0.3 Date of Approval: April 2021 Status: Final Date of Issue: Oct 2023 (version 0.3) Author: Claudia Soiland- Reyes Date of Review March 2024.
The North West has high levels of deprivation. Approximately 1 in 3 (32%) North West residents are estimated to live in the most deprived areas of England, compared to 20% nationally. The most deprived areas include Blackpool, Knowsley, Liverpool and Manchester, with Blackpool, Knowsley and Liverpool’s deprivation score worsening from 2015 to 2019 and Manchester’s score staying similar. However, there are areas with low percentages of people living in the 20% most deprived areas in England, including Cheshire East, Cheshire West and Chester, Cumbria, Stockport and Trafford.
Initial analysis of demand in the 999 (Patient Emergency Service) for 3 months in 2021 shows the following distribution across the five quintiles of deprivation in the population (measured using Index of Multiple Deprivation). This demonstrates the significance of deprivation as a driver for NWAS demand.
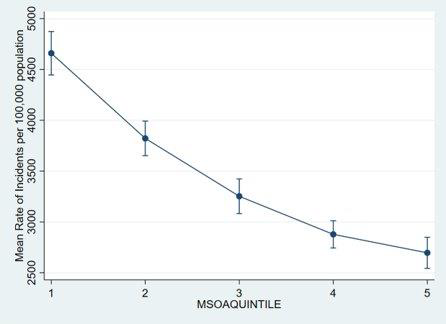
| Most deprived Least deprived |
1.3. Health and disease burden
Overall, the population within the region experiences worse than national average outcomes, such as lower life expectancy, poorer infant mortality and high rates of drug-related death. However, there is significant variation within the region. Life expectancy for females in the North West is 82.1 years (83.4 years for England) and for men 78.4 years (79.8 for England) (data from 2017-19). After years of increasing life expectancy, these figures have begun to fall in the North West overall for the first time, led by reductions in the most deprived areas and plateaus in other areas.
In 2019, non-communicable diseases such as cardiovascular disease and cancer were the main cause of death in the North West (88.95%). Progress is being made in reducing ‘preventable’ early deaths from cancer, cardiovascular diseases and liver disease, though the North West rates are still higher than England. The North West has significantly higher than England average rates of admissions for:
- Alcohol-related incidents or conditions
- Mental health conditions in under-18s
- Self-harm
- Substance misuse
- COPD
- Dementia
- Emergency admissions in under 4s
The COVID-19 pandemic has led to increased mortality in the region, with an estimated 17,868 excess deaths from March 2020 to November 2021. Smoking is still the single largest cause of preventable death in England. Prevalence rates are higher in the NW than in England, though more people tried to quit in 2020. Obesity is fast becoming the primary risk factor of ill health and premature mortality. 67% of adults were classified as overweight or obese in 2018/19 (62% in England). Both these risk factors are more common in more deprived areas.
2. Context
2.1. National context
The NHS Long Term Plan identified the need to reduce health inequalities and focus on prevention. The disparities in outcomes through COVID-19 have increased the scale and pace of this. The 2021/22 priorities and operational planning guidance outlined five priorities for recovery (including workforce wellbeing and avoidance of admissions). The implementation guidance then identified five specific priorities to tackle health inequalities, which includes embedded leadership for health inequalities.
Ambulance Trusts are uniquely positioned to deliver public health approaches due to their high volume of community-based contacts, regional perspective on the health and social care system, rich ‘place-based’ data and insight and specialist workforce. In 2017 the Association of Ambulance Chief Executives (AACE), public health and sector partners published a consensus statement describing the intent to increase collaboration to support improved health and wellbeing among the most vulnerable people in society. In 2021, Public Health Approaches in the Ambulance Sector was published by AACE and Public Health England (PHE) with more detailed proposals. It states that, “establishing senior leadership for the public health and prevention agenda within each ambulance trust is essential”. A national working group, co-chaired by the NWAS Medical Director, is currently updating the consensus statement to identify good practice and produce national recommendations.
The Health and Care Act 2022 gives Integrated Care Systems (ICSs) legal status from July 2022. They are geographically based partnerships that bring together providers and commissioners of NHS services into Integrated Care Boards. Local authorities, Healthwatch and others are statutory partners and make up the Integrated Care Partnership. Integrated Care Boards will co-ordinate and commission health and care services. The proposed changes would also enable providers and commissioners to work closely together through joint committees in local areas. There is an emphasis on the role of provider organisations, especially ambulance trusts, being part of provider system cooperatives to deliver change across the geographical footprint. As with the NHS Long Term Plan, improving population health and health inequalities are key drivers for the proposed changes.
2.2. Local context
Responsibility for public health sits in the NWAS medical directorate with the executive medical director as the lead executive. This work is supported by a consultant paramedic who is the public health lead. In 2020 NWAS welcomed its first Public Health Registrar, funded by Health Education England (HEE), becoming the first (and only) ambulance trust nationally to do this. In 2021, a second registrar joined, and NWAS was awarded HEE funding to appoint a Population Health Fellow.
In January 2021, a Public Health Delivery Group (PHDG) was established to oversee all areas of public health work within NWAS. The group is chaired by the executive medical director and reports to the clinical effectiveness management group (CEMG), a sub-committee of the Trust board. The PHDG will lead on delivery of the public health plan.
NWAS is a member of the Northern Ambulance Alliance (NAA), which was formed to ensure that ambulance services in the north of England are at the forefront of the fast-moving change agenda within both the NHS and wider health and social care system. As part of its commitment to public health and prevention, the NAA supports a lead public health position to align the ambulance service approach to public health across the north.
The new Trust Strategy is clear and bold in its commitment to working with partners to prevent escalating harm and understand and tackle inequalities in access, experience or outcome. It recognises the need to do this to prevent unmanageable demand and improve outcomes for patients and it reflects the interest of staff in this regard, many of whom have led on or become involved with projects in this area.
The implementation section commits in year one to providing an equitable response, working with the wider health care system in the North West to increase referral opportunities and to reducing our carbon footprint. It also commits to further work to plan for year 2 and 3 on:
- Our role in supporting the North West health care system to reduce health inequalities.
- Our roles as a socially responsible organisation.
Public Health Plan Page: 9 Author: Christine Camacho Version: 0.3 Date of Approval: April 2021 Status: Final Date of Issue: Oct 2023 (version 0.3) Author: Claudia Soiland- Reyes Date of Review March 2024
- Understanding how we can widen access into NWAS to increase the diversity of our workforce
The New Health and Social Care Act 2022 mandates new Integrated Care Systems (ICSs) to focus on improving population health and on prevention. Sir Michael Marmot and the Institute for Health Equity are working with each of the North West ICS Population Health Boards and Local Authorities to drive action based on the Institute’s research into the social and economic determinants of health. This supports the on-going development in NW ICSs and some individual Trusts of ‘Anchor Institution’ or social value pledges or frameworks, in which NWAS has shown itself to be an important partner.
3. Public health approaches
Public health approaches prioritise prevention. Using public health approaches within the ambulance sector unlocks the potential to improve population outcomes, tackle inequalities and challenge the demands placed on the sector by preventable causes. The starting point is using data to understand and define our priority areas for action. Evidence can then be used to inform a plan of action. Improvement methodologies can be used to deliver and measure the impacts of changes.
3.1. Using data and evidence to inform practice
A key element of a public health approach is the skilled use and interpretation of data and evidence, to ensure that interventions are as effective as possible. NWAS holds a wealth of activity and call data, which has the potential to make a significant and unique contribution to population health management. We should use our data to explore health inequalities and inform service improvements to minimise inequitable access and outcomes.
3.2. Prevention
Within public health a three-tier model of prevention is often considered, which recognises that there are opportunities to be preventative even after a problem has emerged. An example of primary prevention is the annual NWAS influenza immunisation campaign. This protects our staff and the people we serve from disease. In parts of Lancashire, we have a falls lifting service, which can response to low acuity incidents faster than the standard NWAS response. This is an example of secondary prevention as being on the floor for longer periods following a fall is associated with poorer outcomes. The work our high intensity user team carry out is an example of tertiary prevention. They put support in place for people who often have complex issues and are presenting in crisis.
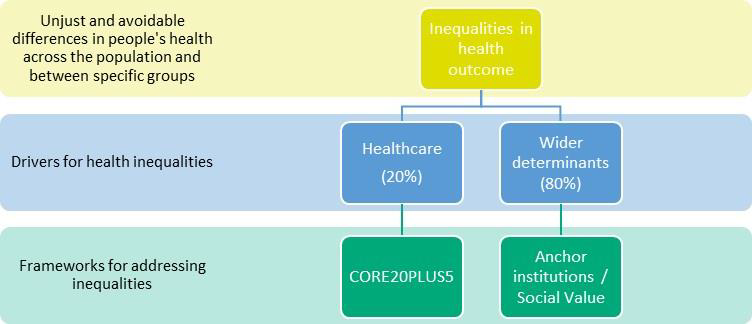
3.3. Health inequalities
The NHS England outlines two roles for NHS organisations with two linked approaches or programmes of work for Trusts and ICSs. These form the basis of many of the Year 2 actions within this Plan:
- Reducing inequalities in healthcare access, experience or outcome (CORE20PLUS5)
- Reducing inequalities in social, economic, environmental drivers of health (Anchor institutions)
The Care Quality Commission (CQC)’s May 2021 strategy commits to looking at how health and care systems are working across partners, including action to reduce inequalities and the 2021 update to the Patient Safety Strategy increases focus on inequalities in experience and outcomes in NHS.
A recent report from The Kings Fund reviews the conditions needed for NHS trusts to make tackling health inequalities ‘business as usual’, pushing care upstream and tackling the underlying causes of inequalities.
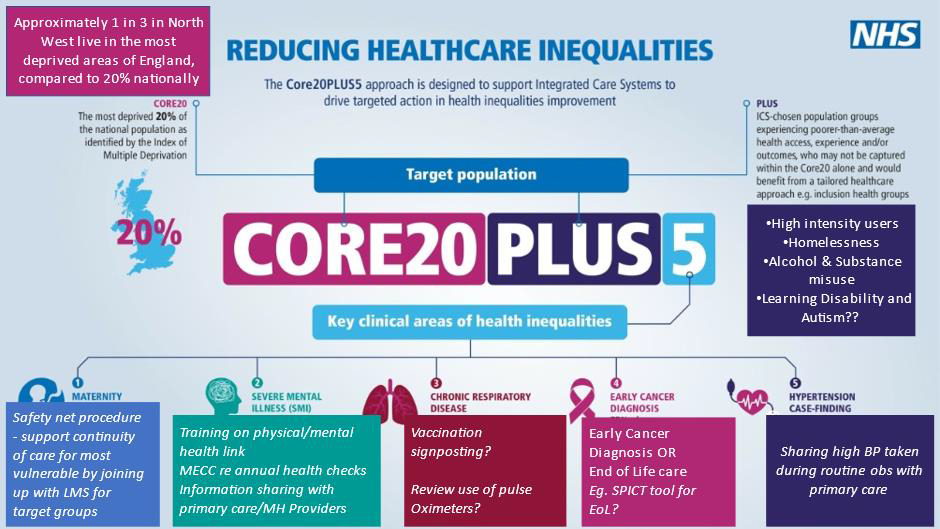
3.3.1. CORE20PLUS5
To drive action in healthcare inequalities (i.e. in access, experience or outcome of NHS Services), NHS England has developed the Core20PLUS5 Framework. It focuses on improvements for the most deprived 20 per cent of the population (core20), reducing inequalities for particular population groups identified locally (plus) and accelerating improvements in five clinical areas (5).
The Public Health Team within NWAS have begun to interpret this for the Trust to consider where we can have the most impact. Specific actions are included in the relevant section of the Plan under Year 2 updates and summarised below in an adapted version of the National graphic:
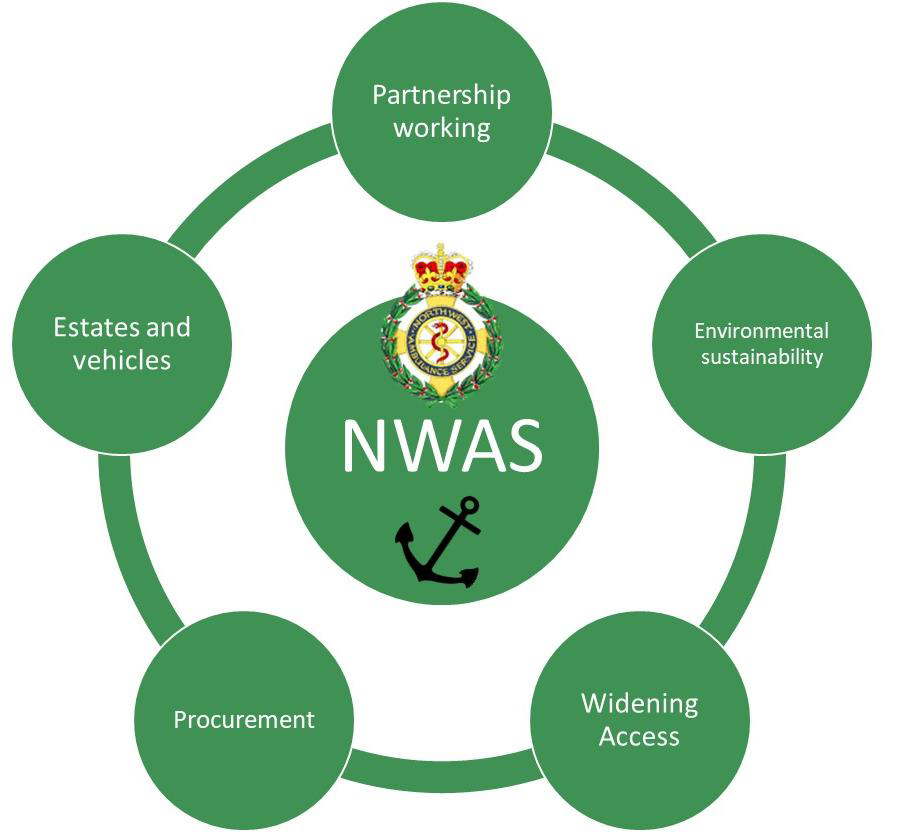
3.3.2. Anchor institutions
To contribute to addressing wider determinants of health (or ‘causes of the causes’), the NHS Long Term plan asks NHS organisations to recognise the significant economic, environmental and social value impact they can have as ‘Anchor Institutions’; that is large providers, consumers and employers in their communities. The Health Foundation identifies 5 ‘pillars’ through which NHS organisations impact communities (see diagram below, adapted for NWAS).
In January 2022 NWAS Public Health Delivery Group hosted a workshop with NHS E/I NW, AACE and the Office for Health Improvement and Disparities (DoH). National events and discussions are on-going to develop sector-specific frameworks and commitments.
NWAS have recognised this aspect of the Trust’s role in the new Corporate Strategy, particularly around workforce, environmental sustainability and procurement for social value and recognises the need to work more closely with ICS partners. The year two actions in this Plan support NWAS to develop an accurate baseline and articulate its ambitions, with progress measures. The Trust’s Green Plan (v2, 2021) uses the Sustainable Development Assessment Tool every 6 months to monitor progress in 10 key domains which cover much of this work. The SDAT Framework is being reviewed, providing an opportunity to re-articulate the Trust’s sustainability approach, in its broadest sense.
3.4. Partnership working
The health and wellbeing of the population is the shared responsibility of a wide range of sectors, including health, social care, Government, the voluntary sector, education, and many more. A key public health skill lies in influencing the use of time and resources in a collaborative way that improves population health and wellbeing. Public health approaches are always consciously located within a wider system rather than thought of in isolation. The incoming changes around commissioning function of ICSs and the role of provider organisations in improving population health provide opportunities for NWAS to strengthen its influence in the region.
3.5. Research
Public health approaches in the ambulance sector are an emerging area and as such there a dearth of peer reviewed research in this field. Evidence based practice is an important means to improve clinical practice, however for public health approaches specific to the ambulance sector there may be insufficient scientific literature to inform the basis for clinical decisions. In line with the NWAS Research Strategy, we must consider our research output for public health; we will seek to establish research priorities which align to the needs of our organisation as well as the wider ambulance sector. We will endeavour to engage in the production of high-quality research in the Public Health field and share our findings through recognised channels to raise the profile of our public health work and share our learning with other ambulance services.
4. Embedding public health approaches in NWAS
Four priority areas to support the organisation in embedding public health approaches have been identified. In November 2021– March 2022 a review of year one activity was undertaken. As well as desktop review, a survey was shared with staff and various sessions were held on public health in NWAS. Feedback through consultation on the Quality Strategy and the Corporate Strategy also informed the review and production of year two actions. This section presents an overview of work achieved in year one and milestones agreed for year two for each of the 4 sections depicted below.
4.1. Strategy
Where are we now?
The new Trust Strategy is clear and bold in its commitment to working with partners to prevent escalating harm and understand and tackle inequalities in access, experience or outcome. It recognises the need to do this to prevent unmanageable demand and improve outcomes for patients and it reflects the interest of staff in this regard.
Where do we want to get to?
Public Health should be embedded into the Trust’s core business through input to each of the enabling strategies and implementation plans. The implementation section in the Trust Strategy commits in year one to providing an equitable response, working with the wider health care system in the North West to increase referral opportunities and to reducing our carbon footprint. It also commits to further work to plan for year 2 and 3 on:
- Our role in supporting the North West health care system to reduce health inequalities
- Our role in the system and responsibility as a socially responsible organisation
- Understanding how we can widen access into NWAS to increase the diversity of our workforce
Year 1 Milestone progress
PH Team were on Right Care group. Current draft includes reference to inequalities
Includes some specific clinical groups which align to CORE20PLUS5
Additional work delivered in year 1
Public Health Delivery Group established and grown
PH involved in Corporate Strategy throughout – content reflective of PH priorities
Extensive national and regional engagement
Mapping of ‘Anchor institution’-related activity (social value role)
Board Development Session
Aims, Objectives, Logic model and review of year 1 developed
Regular PIMS – PH Liaison
Year 2 milestones
Produce Comms and Engagement Plan for quarterly review of key messages. Include:
Engagement with national bodies on public health / health inequalities in the Ambulance Sector
Membership of ICS Population Health Boards
Membership / links to NW Healthcare Public Health Network
Provide Public Health input to Corporate Strategy Implementation Plan and enabling strategies
Outline NWAS’s role in tackling Health Inequalities, including: CORE20PLUS5 Action Plan (Inequalities in Health Care)
Baseline measurement framework for NWAS as an Anchor institution / Social Value
Gain Cheshire & Merseyside Social value award (recognised across NW) including action plan for future years, in line with Green Plan.
4.2. Data and intelligence
There is an opportunity to develop the use of internal data to improve a targeted and preventative focus, and to contribute to a ‘population health management’ approach across the wider integrated care systems that we operate within. There is also an opportunity to make better use of the wider population health and wellbeing data available through our external partners, to further inform prioritisation and planning.
NHS Planning Guidance and the CORE20PLUS5 Framework highlight the need to collect accurate data on patient characteristics and pro-actively delineate performance and demand data in order to target, prioritise and provide assurance of equity.
Where are we now?
NWAS has begun work to improve ethnicity data recording in the emergency service (PES), building on high levels of completion in 111 and PTS. Dashboards have been produced this year to support Mental Health, Falls and Maternity programmes. These can now be developed to monitor inequalities more closely.
We currently have no public health analyst capacity in the organisation. The lack of knowledge and skill in this area will be a blocker for us progressing the more advanced analytics sprints which we will want to conduct in later stages of this stream.
Where do we want to get to?
In order to fully support our public health objectives, we must have the right data and intelligence solutions in place.
Year 1 milestone progress
Design and deploy a public health dashboard, with data on at least 1 topic of interest which combines internal and external data sets
Mental health, falls dashboard and maternity dashboard developed.
Public health dashboard not developed due to backlog in Informatics (though individual projects supported).
Review requirements and informatics capacity (inc data warehousing) to support year 2/3.
Additional work delivered in year 1
Analyses of inequalities and epidemiology – OHCA, falls, demand, HIU presented to relevant Boards and supported follow up
Accident Prevention – investigation and coordination of prevention activity and escalation
Year 2 milestones
Existing dashboards (mental health, falls, maternity) to be disaggregated by ethnicity and deprivation
Produce analyses to support CORE20PLUS5 action plan working with NIHR-CRNs and ARCs as research partners Identify at least 2 PLUS Groups of relevance and develop mechanism for capturing interaction with NWAS (eg. fields in ESR / audit / Research etc)
Develop demographic analyses of 5 Clinical areas in CORE20PLUS5
Share OOH Cardiac Arrest analysis and proposals with Clinical SMT and external stakeholders to inform system improvements
Test a pro-active ‘surveillance’ approach within new major incident cell to inform move towards syndromic surveillance mechanism.
4.3. Building capability
The public health consensus statement supports a commitment to ensuring that the paramedic workforce is fully equipped with the skills, knowledge and attributes to promote the health and wellbeing of individuals, communities and populations. The College of Paramedics includes public health within its defined scope of paramedic practice, supporting recognition of genetic, environmental and social influences of disease and ill health, and the application of the principal of health promotion and disease prevention.
Where are we now?
Some public health training is included in undergraduate training for paramedics. There is no NWAS mandatory training specific to public health. Although the milestones were not delivered in year one as originally envisaged, a lot of work has taken place to share fundamental public health knowledge and support those with an interest to lead projects and help shape the programme, thereby supporting the corporate goals to make NWAS a desirable place to work and a Trust constantly striving to improve. The extent of support for staff to identify and undertake further development opportunities such as Apprenticeships, Advanced Practice, HEE Population Health Fellowships depends on the Public Health Leadership capacity available (see Risks 2.3 above). There are some development programmes, tools and networks available already which NWAS workforce could access, though these are not well known and some need adapting for the sector.
Where do we want to get to?
Our vision is for NWAS employees to be competent and confident to support public health approaches and be supported by the Trust to do so. Three ‘tiers’ of skills and knowledge and resource are needed: fundamental knowledge and skills such as confidence in behaviour change conversations for the front-line; advanced skills and support to lead quality improvement projects for those with more interest or experience and relevant roles; specialist public health leadership capacity including analytics.
Year 1 milestone progress
Develop a framework to assess public health knowledge and skills in the organisation
Identified resources with HEE, PHE/ OHID but not rolled out
Advised to develop language, interest, networks first
Additional work delivered in year 1
Applied to host and recruited to HEE Fellowship with significant strengthening of the PH team
Trauma-informed training
Staff engagement activity
Year 2 milestones
Develop NWAS Public Health workforce: Employ Public Health Manager (Band 7)
Develop Business Case and Job plans for Public Health Consultant and Public Health Analyst on test of concept basis
Public Health input to NWAS Leadership for Inclusion module
Develop capacity building arrangements with NW PH Knowledge Intelligence Services (through NHS E/I, OHID and LAs)
4.4. Supporting delivery
A Public Health Delivery Group (PHDG) was established in January 2021. Chaired by the Executive Medical Director, the purpose of this group is to provide strategic oversight for the Public Health Plan and support the delivery of public health initiatives in the organisation.
Where are we now?
There is no funding allocated to prevention which is a barrier to rolling out initiatives across the NW. Delivery is patchy and dependant on individual CCGs or LA commissioning services which NWAS may be a delivery partner in. The year one review highlighted progress through specific projects, often led by staff going beyond their ‘core’ role or using their own time. The involvement of front-line staff is positive but an over-reliance is not sustainable or consistent so this must be considered in the process of the SDMR and discussions with commissioners.
Where do we want to get to?
Our vision is to have new commissioning arrangements in place which support NWAS in delivering public health initiatives across the NW and to have capacity to identify and influence external funding opportunities. This may be assisted by implementation of ICSs and /or national commissioning for some aspects of the Trust’s business as well as improved relationships with wider healthcare public health and local authority partners.
Year 1 milestone
Discussions with lead commissioner and 4 STPs on NWAS role in delivering public health.
Discussions with clinical and QI lead from Blackpool CCG, supportive of public health approach.
PIMS team engage ICSs with support from PH Team and others.
Mapping of social prescribing referral pathways.
Social Prescribing Working Group established
~20 pathways now in place.
Significant work on information governance, pathways and digital integration. Model to follow for other projects / pathways.
Additional work delivered in year
Violence Prevention programme – hosting Youth Navigators; delivery of Street Doctors programme to young people, with NQPs
999 ReUnite scheme for patients Alzheimer’s
Mapping falls pathways and services
Year 2 milestones discussions
Delivery of CORE20PLUS5 action plan: Maternity – Test improved join up / info sharing for vulnerable cohorts (PES and 111)
Increase awareness of physical health needs for patients with Serious Mental Illness; embed MECC approach to improving take up
Hypertension – Pilot sharing high Blood pressure data with primary care
Consult on at least 1 other clinical area of focus involving 111 and PTS. (Eg. chronic CORE20PLUS5) or falls / frailty / Dementia/ End of Life care as local alternative
Utilise analysis / research into PLUS groups to develop proposals to improve access, experience or outcome eg. naloxone referral for opiate users or homeless patient outreach
Violence Prevention Programme: Secure funding to deliver ‘Street Doctors’ sessions in Colleges, with NQPs
Develop research proposal to embed and evaluate trauma-informed practice programme in one area
Embed Oasis YP Navigators pathway and support referrals
Develop Business Case for programme support and staff backfill
Review learning mechanisms and embed NHS Patient Safety Framework to utilise population-level analysis of harm and allow pro-active learning
Continue to embed social prescribing pathways and review learning for other pathway development
4.5. Overview of year 2 milestones
Year 2 Milestones
Strategy:
Produce Comms and Engagement Plan for quarterly review. To include up to date USP / key messages and: Engagement with national bodies on public health / health inequalities in the Ambulance Sector NWAS membership of ICS Population Health Boards Membership / links to NW Healthcare Public Health Network and Place-based PH leads
PH Lead / Comms / PIMS Medical Director / PHDG Regional Director / PIMS NWAS PH Lead
Provide Public Health input to Corporate Strategy Implementation Plans and enabling strategies
NWAS Public Health Lead / PHDG / Head of Strategy
Outline NWAS’s role in tackling Health Inequalities, including: CORE20PLUS5 Action Plan (Inequalities in healthcare). See: NHS England » Core20PLUS5 – An approach to reducing health inequalities Baseline measurement framework for NWAS as an Anchor institution / Social Value Gain Cheshire & Merseyside Social value award (recognised across NW footprint) including action plan for future years, in line with Green Plan.
Head of Informatics
Data and intelligence:
Produce analyses of data to support CORE20PLUS5 action plan (see 3. above), working with NIHR-CRNs and ARCs as research and data partners: Identify at least 2 PLUS Groups of relevance and develop mechanism for capturing interaction with NWAS (eg. fields in ESR / audit / Research etc) Develop demographic analyses of 5 Clinical areas under CORE20PLUS5
Public Health Lead / Clinical Leads / Aps / CSPs / Masters Students etc Informatics with CORE20PLUS5 Project Leads / Research Team
Complete Out of Hospital Cardiac Arrest area analysis (Oct 22). Share with Clinical SMT, NWAS Community Resus Team and other internal stakeholders. Investigate application to defib development work. Develop links with external stakeholders inc Cardiac Networks and LA Public Health Leads.
Population Health Fellow (CM)
Test a pro-active ‘surveillance’ approach within new major incident cell to inform move towards syndromic surveillance
Major Incident Cell / Clinical Effectiveness Lead
Building capability:
| Develop NWAS Public Health workforce: Employ Public Health Manager (Band 7) Develop Business Case and Job plans for Public Health Consultant and Public Health Analyst on test of concept basis | Medical Director / Workforce Director Public Health Lead(s) |
| Building public health knowledge and skills (with HEE, AACE, OHID support): Incorporate PH content into mandatory training and CPD Deliver at least 3 PH training sessions for NWAS staff and record one session for open access | Public Health Lead(s) / CP Education Public Health Lead(s) supported by PHDG |
Supporting delivery:
| Delivery of CORE20PLUS5 (Health Inequalities) action plan: Maternity – Test improved join up / info sharing with services for vulnerable cohorts (PES and 111) Increase awareness of physical health needs for people with Serious Mental Illness; embed MECC approach to improving take up of annual health check Hypertension – pilot sharing high blood pressure data with primary care Consult on at least 1 other clinical area of focus on inequalities involving 111 and PTS. Consider chronic respiratory illness and early cancer diagnosis (as per CORE20PLUS5) and explore falls / frailty / dementia / End of Life care as local alternative Utilise analysis / research into PLUS group to develop proposals to improve access, experience or outcome eg. naloxone referral for opiate users | Consultant Midwife Mental Health Lead Nurse Public Health Lead / PIMS / Transformation NWAS Public Health Lead / PHDG Public Health Lead / Quality Team / Research Team / Evaluation Lead / Others |
| Violence Prevention Programme: Secure funding to deliver ‘Street Doctors’ sessions in Colleges, with NQPs | AP Violence Prevention |
5. Summary and review
This plan outlines the Trust’s ambition to embed public health approaches across the organisation. Prevention and population health management feature strongly in national policy. Proposed changes to NHS commissioning and the role of providers provide an opportunity for NWAS to play a more central role in the region. Strengthening our public health delivery will help the Trust achieve its vision of being the best ambulance service in the UK by delivering the right care, at the right time, in the right place, every time.
The year 2 milestones will be reviewed in Quarter 4 of 2022/23 to consider learning, change in context, staff feedback and to develop future year(s)’ milestones. Milestones for year 3 will be agreed by the Public Health Delivery Group.