Community Listening Event Report 2023-2024 (2MB pdf)
On this page

Introduction
This report provides a summary evaluation of feedback and themes from the North West Ambulance Service (NWAS) five community listening events, successfully delivered in each county across the region between October 2023 and March 2024. The events were delivered by the trust’s Communication and Engagement Team, supported by front line colleagues and senior management.
Background and Context
The main aim for us holding the events was to engage with and listen to local communities, particularly those that are often under represented. We also wanted to improve awareness and access to ambulance services; paramedic emergency service (PES), NHS 111 and patient transport service (PTS). In Cheshire, where we do not currently hold the PTS contract, this was replaced with information on our Emergency Operation Centre (EOC).
We held similar events in 2019-20 and 2022-23. The 2020-21 and the 2021-22 events were cancelled due to the COVID-19 pandemic.
The initial format for the 2023-24 events was similar to the ones held in 2022-23; three lightning talks (five minute presentations), followed by informal-facilitated exercises for attendees, and a question and answer session to close the event. We were able to use feedback from attendees, and the team’s experience, to modify the activities and event structure for the 2023-24 events. This is detailed in section 7.1 below.
One key addition was the inclusion of how we had used feedback from the community at the previous year’s events to improve services.
Service improvements based on 2022/23 events feedback
In Lancashire one attendee told us: “It would be useful to know the estimated time of arrival for an emergency ambulance when you call 999”. As a result of this feedback, we have started to inform patients of the estimated time of arrival for an emergency ambulance. Other feedback shared with us by the Lancashire Council of Mosques encouraged us to remove any photos with faces on them from promotional materials so they can be displayed in mosques, allowing us to reach a wider community audience.
One of the issues brought up by attendees at our Greater Manchester event was that some ethnic communities were not aware of the services provided by NHS 111, as well as who can use PTS, or the requirements for eligibility. All our community listening events include dedication sections on both services (except for PTS in Cheshire) and since receiving this feedback, the Patient Engagement Team has made sure we talk about these two services when we attend high footfall community engagement events across the North West. The team has actively developed new relationships with mixed ethnic community groups to help improve understanding. We talk about how to access the service, dispel any myths, and explain how the service works and how it might help them in the future. New materials have also been produced to support this engagement including an A-Z of PTS services launched in February 2024 and a new A-Z of NHS 111 services about to be published in summer 2024.
At our events in Cumbria and Cheshire last year, a recurring theme we heard from those who attended was that some Deaf groups are unaware of what the NHS 111 service can offer as well as how they can access our service. Since receiving this feedback, we have been met with various Deaf groups across the region to inform Deaf patients how they can access our services through communicating via British Sign Language (BSL). We have since launched the Insight app across the trust which allows our 999 and PTS crews to communicate via an interpreter. We have also developed easy read guides for our three core services which are available on our website and we have refreshed our pictorial handbook which will shortly be launched and is used by ambulance crews on trust iPads with patients when needed.

Attendees
We aim to attract a wide range of attendees as possible by using our community contacts and networking. In total 318 individuals booked on to the 2023/24 programme of community listening events, with 202 (64%) attending overall.
This compares positively to the 193 who attended the 2022/23 events. 67 (33.2%) of the 202 attendees belong to ethnic minorities and 29 (14.4%) of the 202 were identified as having an accessibility need through the booking form.
54 overall groups and organisations attended the five events which can be grouped into 18 different types including, NHS, community specific, learning disabilities, support groups and religion (see table 1).
We ask participants to indicate special dietary requirements and accessibility needs on the booking form, for example additional facilitator support and/or a BSL interpreter.
| Group type | How many groups | How many individuals per group |
| Age UK | 2 | 2 |
| Cancer | 1 | 1 |
| Carers | 3 | 9 |
| Community specific | 6 | 7 |
| Council | 1 | 5 |
| Culture | 2 | 15 |
| Disability | 3 | 14 |
| Education | 2 | 2 |
| Employment | 1 | 1 |
| Gender | 1 | 1 |
| Healthwatch | 1 | 3 |
| Learning disabilities | 4 | 13 |
| Medical | 3 | 3 |
| Mental health | 1 | 1 |
| NHS | 7 | 9 |
| Support groups | 4 | 7 |
| Religion | 4 | 8 |
| Volunteers (PPP, CFRs, VCDs) | 3 | 31 |
Accessibility needs of the attendees
At our event in Lancashire, members of the Deaf Village, a Deaf-led organisation that promotes inclusivity, attended and brought their own BSL translators. They commented on the challenges of translating written English into BSL and the additional time needed to accomplish this. We’ll investigate how the 2024/25 events can be adapted to support this.
We had two attendees at the event in Greater Manchester: one was registered blind, and the other had a significant visual impairment. They asked for copies of the agenda, materials, and/or presentations to be emailed to them ahead of time so they could review it beforehand and follow along on the day, just like everyone else. Since one of the videos planned for use at the event had only music playing in the background, the team opted to remove the film from the agenda.
We had a guest at out event in Cheshire who didn’t disclose their visual impairment on the booking form. We made sure they could fully participate on the day, and after the event, we sent them the slides to review.
Listening and engaging
The dates and locations for all five community listening events were as follows: Liverpool (Merseyside) 26/10/23, Blackburn (Lancashire) 23/11/23, Cheetham Hill (Greater Manchester) 23/01/24, Carlisle (Cumbria) 22/02/24, and Northwich (Cheshire) 05/03/24. We have revisited some of the venues from the last series of events, following successful experiences at these venues. For the 2023/24 events, we scoped new venues for Merseyside and Greater Manchester.
Activities
Paramedic emergency service
Initially, when facilitators announced the name of a subject, participants were asked to write down the first word that sprang to mind. Facilitators then discussed the words chosen. Directly after the event in Merseyside, we adapted the activity to focus on the reasons and expectations of why people call 999 to gather more insightful feedback. For the new activity, we asked to hear the three primary reasons they would call for an ambulance as well as their expectations of the service they would receive if they were to make this call. The reasons and expectations shared were then discussed. If falls as a topic in general was not mentioned, facilitators were asked to raise it as a discussion point. Discussion of falls services and how we respond to this frequent type of incident was added to help support this element of education and awareness raising as part of our winter demand management campaign for 2023-2024.
NHS 111
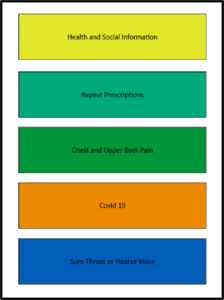
Each table had five buzz cards with the top five symptoms for which patients contact NHS 111 (figure 1). We requested participants to arrange them according to their perceived ranking in relation to issues attracting the greatest number of calls. Facilitators would reveal the correct order and discuss. Again, this activity supported increasing awareness of what services NHS 111 can provide but also where best to go for particular forms of care or assistance as part of the winter demand management campaign.
Patient transport service
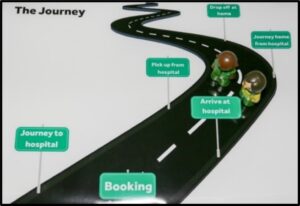
We asked participants to consider every aspect of the patient journey and tell us what they thought would make an excellent patient experience. Key ideas were written on ‘post-it’ notes and stuck to the roadmap around the relevant heading (figure 2). Feedback from this activity was used to help inform our A-Z of patient transport services.
Emergency operations centre
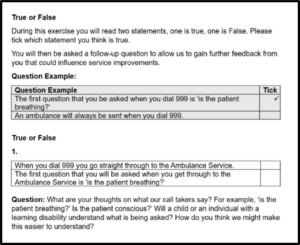
We gave each attendee an activity sheet and asked table groups to consider different aspects of calls to the EOC, specifically what they believed would make an excellent experience. Each question had two statements, one which was true and one which was false. Each attendee had to tick which one they believed was ‘true’. There were follow up questions to gain further feedback to assist in making appropriate changes moving forward (figure 3).
Question and answer session
Attendees had the opportunity to share any questions or comments about the event, or out services, by using the A5 sheets we provided with empty speech bubbles (figure 4).
The questions were then answered by the Deputy Chief Executive, Salman Desai or other managers in the room. Post-event, all the questions and comments were collated to look for key themes.
What we heard from attendees
The feedback themes shown below were collated from the relevant service line activity.
Paramedic emergency service (PES) feedback
Accessibility
- Senior people often won’t ring 999 and don’t know about the 111 service. Some people similarly won’t use anything in the community/pharmacy etc. and expect to self-recover but can often then deteriorate.
Information/communication/education
- BBC programme raised awareness on why people ring 999 and how paramedics don’t need to attend every job (e.g. falls, can’t get up but no one to help, not injured and not in pain).
- More education needed in the community, simple prevention information.
- Discussed the difference between paramedics and emergency medical technicians.
- Public perceptions of ambulance service always meaning paramedics but this is not always the case.
- Expectations – lack of education – this needs to be started early in schools.
- You expect an ambulance for anything you couldn’t deal with yourself e.g. older individuals who fall and can’t get up.
- Community first responders (CFRs) – not heard of this service before, how long have we had that in place? What type of incidents do CFRs attend?
- People think if an ambulance takes you to hospital, you get bumped up the queue. This is a myth. You will be triaged based on your medical needs.
- Education at all ages, what the service is there for. Younger people would like lessons. More senior people are more traditional, need doctor, ring doctor, anything bigger 999 when they might not need 999. Not sure what service to ring.
- Better health promotion to help public in need or preventative information.
- Mental health calls – what is our response to a crisis call?
- Could call handlers FaceTime to see the patient?
- Why do ambulances attend some people quicker than others?
- The view that people abuse the ambulance service.
- What is the percentage of inappropriate calls?
- Different perceptions of response time – what is classed as a fast or slow response?
- Can we call people back if there are delays with an ambulance?
- Good to give patients an approximate idea of wait time.
- Moving notice board (like in GP surgeries with how many missed appointments) – NWAS version.
- Online advert? On phones/games – how much would this cost?
- Mental health crisis – don’t know about other numbers. 999 is known and accessible and they know they will get help.
- Perception of ambulances waiting in stations.
- Is there a community service to support patients?
- Want honesty on the phone, reassurance, help due ASAP but aware of ‘can’t say time frame’ for ambulance involved.
- Struggle with GP appointments – puts strain on other services.
Experience
- Rang ambulance, someone knocked themselves out, called ambulance, one in area, came very quickly. First class response, very professional.
- Still went through questions even though they knew the patient was having a stroke.
- Discussed personal experiences and how expectations need to change.
Falls
- Falls – attendees were impressed by the specialist equipment that medics have.
- Discussed falls awareness, at what point do the elderly need an ambulance? Senior people often fear this will be start of their decline.
- Use Community Response Service (CRS) for falls. Device to help people back up to standing, saves paramedic response.
- Falls – correct moving and handling technique.
- Falls – age dependent (if older, immediate response). Quality of life in older people falling impacting later on with mental health and dementia.
- It was discussed that when a relative falls at home, that they would contact 999 with the expectation that the person who has fallen is treated or aided to their feet.
- Conversation around why patients are left on floor – how to make time on the floor shorter after fall.
- Less support in the system if fallen: what to do, where to do, what help is available?
NHS 111 feedback
Accessibility
- The internet can be a barrier to information for those who don’t have access or know how to use it.
- People who use BSL find NHS 111 online difficult to use because written information is not translatable in the same way as BSL.
Information/communication/education
- People don’t know the full scope of other services e.g. pharmacy.
- Additional messaging around prescriptions – bank holidays etc. Not always timely enough – most pharmacies take a week to process now.
- What is NHS Choices?
- Maybe there should be more promotion of NHS 111 so people can understand all the services that are on offer.
- Lack of NHS dentist services was discussed.
- Wonder how much money the repeat prescription service has saved the NHS.
- Group didn’t realise how many calls to NHS 111 are related to health and social care/signposting.
- Feel that information is available, but people don’t look for it.
- University students ring NHS111 for repeat prescriptions when they are away from home, can we put information out about how to access a GP.
- People may call the service, because they are lonely.
Experiences
- Feedback from NHS 111 from someone who used to manage a care home – of all of the services, NHS 111 is the most disappointing, length of wait time, appears that advisors are ‘ageist’ (if over 75, told to wait until Monday to contact GP).
- ‘Unhappy with time it all took’ – 45 minute triage, 45 minutes again then over five+ hour wait for an ambulance.
- Experience – sent to pharmacy who didn’t have the medication needed.
- Called NHS 111 because new in the country and not sure which number to call/worried about breast feeding.
GPs
- Route to access services (quicker to go through 111 than to go through GP).
- Conversations around GP availability, antibiotics, COVID-19, post-pandemic issues.
- Do people ring NHS 111 for prescriptions due to people being unable to see a GP?
- People can’t get through to GP so will call NHS 111.
- ‘Loophole’ to get GP appointment – GP appointments available.
- GPs easily signpost to 999 when not the most appropriate ‘fob off’.
Patient transport service (PTS) feedback
Accessibility
- Journey – can be language barriers.
- Booking – online discussed but acknowledgement this isn’t accessible for all.
- PTS – not well known by ethnic minorities.
- Discussion over GPs not telling patients about the PTS service.
- Accessible – would need to be in BSL as that is their first language, not English.
- Low immunity – can I use this service? Is it appropriate? Can I request a car instead? How can I book this?
- Lots of discussion about deaf people’s experiences of using PTS.
- Accessibility for neurodivergent – friendly, calm, polite.
- No acronyms, plain ‘English’.
- Difficulty taking wheelchairs and frames.
- Enhanced users (cancer/renal patients) – can’t share with other patients.
Information/communication/education
- Vehicle banner – promote messaging to raise awareness of how to use the service.
- Awareness of not over-relying on PTS.
- Volunteer car drivers – who are they and how do they apply?
- Can volunteer services/local councils provide a budget to help promote PTS.
- Questions around eligibility for PTS (discharge after elective c-section)? Do midwives know about PTS, and would they highlight this to patients?
- PTS staff are sometimes mistaken for ambulance crew which affects the expectations of our users.
- Can the nursing staff book my journey home?
- How long will the journey take? What about delays on roads or motorways etc.? Don’t want to be late.
- Can I take my family with me (or friends)?
Experiences
- Accessible vehicles – Wheelchair accessible vehicles? Not accessible to take own wheelchair or scooter.
- Taxi’s do not take to appointment place, just hospital grounds.
- Why be ready two hours in advance and awaiting return?
- When getting picked up, waiting a long time for others too can be challenging if many people in ambulance.
- Eligibility could be simpler. Users sometimes get confused by the questions, very scripted.
Expectations
- Taking to the doors/department is very helpful and needed.
- Journey home – discussion around the time it takes to get home potentially being longer.
- An answer/call back system for booking.
- Making sure people are safe when home, not just dropped at door.
- Description of who’s picking them up (uniform), type of vehicle (non-emergency ambulance) etc.
- Drop off home – good opportunity to evaluate home environment, support needed etc.
- Drop off – especially in the dark, don’t want to go in by themselves. Might not feel safe.
- Do staff have access to medical records?
Suggested improvements
- Text would be good to help let the patient know when they’re arriving.
- Very helpful to have tracking and visuals like an Uber taxi app.
- Provide a map to all PTS – standardised map with central points for drop off and collection.
- Do we send out questionnaires? Could we get people to do the surveys with the patient i.e. the driver.
- Tracking system to update patients.
- Are there links with ‘Ring and Ride’? Why not?
Emergency operations centre (EOC) feedback
Information/communication/education
- Participants were unaware of being connected to BT first.
- Were aware of the category of calls but thought some incidents might have ranked higher.
- Do not feel being informed of the category would be helpful. Agree it would be more helpful to be informed of the time frame to expect for a response.
- Misunderstanding about staying on the phone line until arrival of ambulance. Facilitator explained why this happens and why callers will be released if non urgent.
- Phone caller at EOC and dispatch are working on your call, whilst on phone to patients. The public think ‘their call is taking up call time from other calls, or don’t realise the staff working on the call in the background’.
- Public sharing of awareness – the need for an ambulance or PTS vehicle so they can be where they are needed. Public can either wait for ambulance, or travel by taxi/friend/family if able.
- Keypad/lockbox code for gated community can be given.
Accessibility
- Discussion about difficulties a child or individual may have about recognising an unconscious patient, may believe they are asleep, need to consider the questions we ask.
- Suggested different scripts for younger callers or patients with dementia.
- Talked about using mobile phone video, facetime feature to give the call handler visibility of the incident.
- Artificial intelligence has greater input to independence, helping by phone activation by voice for disabled and sight loss support. Otherwise, they would struggle with supporting and using phone.
- Discussion on community defibrillators – access, how to find them, and codes to release the machines. Scared to use if unfamiliar. Sight loss can make it hard to see/push buttons etc.
Question and answer key themes
A few of the queries raised by attendees are already included in the above section. Other questions included:
Paramedic emergency service
- How do you categorise emergencies?
- How are you managing the long waits for ambulances waiting for lengthy periods at hospitals?
- Do all parts of North West have falls and MH cars?
- “Falls support services” – Who are they? Where are they?
- How are you developing inclusivity for BSL users when using 999 and 111 services?
- How can you better promote health advice to the public, to get the right care at the right place? (e.g. what to do with a cough, cut, medical support if needed ASAP). The public doesn’t seem to know when to call 111 or 999.
- Do GP/hospital/ambulances communicate effectively re-being able to see records?
NHS 111
- How many NHS 111 calls get diverted to 999?
- NHS 111 online is difficult for people who use BSL to translate. Is there an option to use BSL NHS 111?
Patient transport service
- For patients with permanent medical issues, i.e. double amputee with conditions, why isn’t this able to reduce eligibility questions and have details held on file?
- PTS – how do you support patients with dementia?
- How do you promote accessibility in terms of neurodiversity to ensure ease in booking and travel?
Emergency operations centre
- If someone was to ring 999 and their call was cut off, would you be able to call them back if their number was withheld?
Careers
- If I want to become a paramedic, how do I? Where can I get information?
Event evaluation
At the end of the event, all attendees were given the chance to complete an evaluation form to give feedback.
The first question asked for three things attendees liked about the event and the second for three things that could be improved. These are all non-prescriptive, open questions where attendees could comment on the venue, event, food, or networking opportunities or anything else to avoid leading or prompting particular responses.
The recurring themes indicated that attendees enjoyed how informative the day was, the opportunity to network, and the interactive activities the most. Other suggestions include inviting other emergency services (police, fire etc.) to be part of the event, allow more time for discussions and provide more volunteer and recruitment information.

What an interesting morning spent with the North West Ambulance Service team. Hearing about the community opportunities and offers they deliver. Wonderfully organised (and free bite to eat too) with some great networking with local people!
Cumbria Oddfellows
We always appreciate hearing feedback like this from the Oddfellows in Cumbria about their time at our event in February.
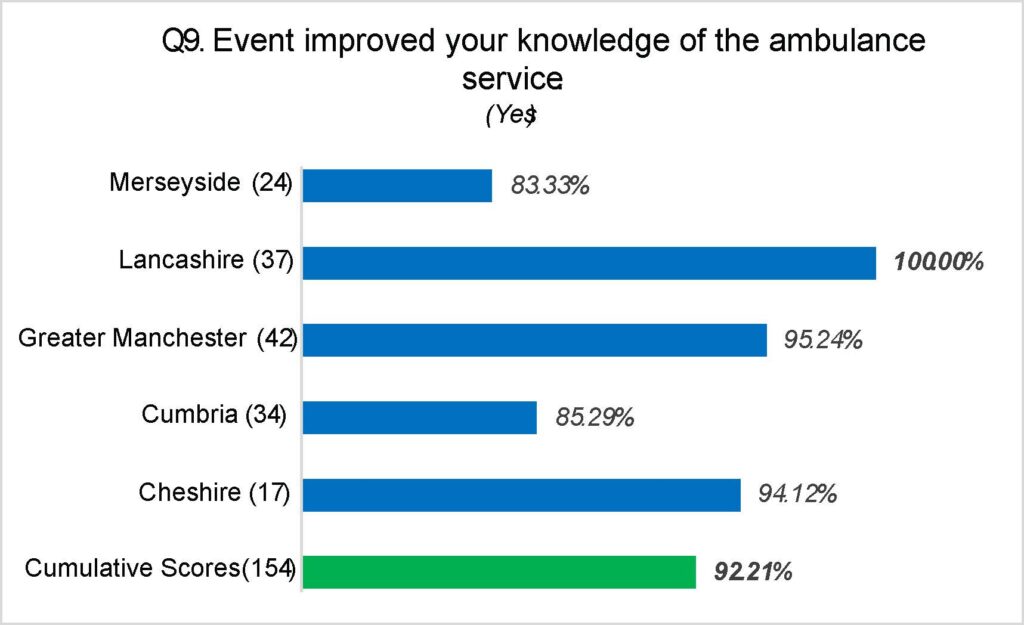
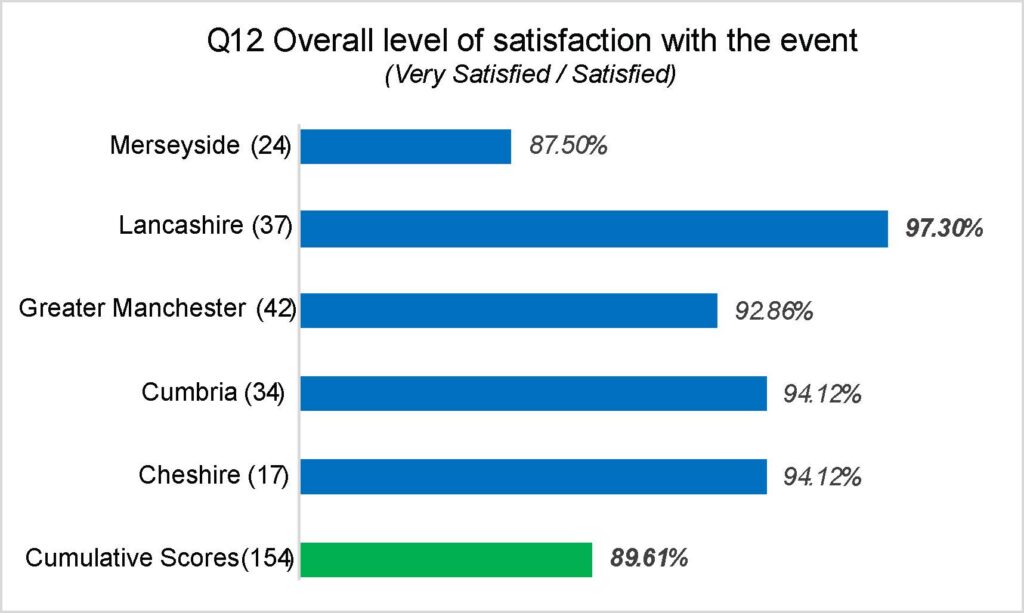
As shown in table 2 and graph 1, 92.21% of all attendees felt the event improved their knowledge of the ambulance service. Cumulatively, 89.61% of attendees were overall ‘very satisfied’ or ‘satisfied’ with the event they had attended, a 0.99% increase from the 2022/23 events. It’s important to note that the level of overall satisfaction at the events increased after we made changes, following feedback (graph 2).
| Questions | Merseyside | Lancashire | Greater Manchester | Cumbria | Cheshire | Cumulative scores | Cumulative scores 2022-2023 |
| How would you rate the organisation of the event? [Very good/good] | 100% | 100% | 100% | 94.1% | 100% | 98.1% | 98.7% |
| How helpful were the event team? [extremely helpful/very helpful] | 95.8% | 97.3% | 92.9% | 94.1% | 100% | 95.5% | 100% |
| The duration of the event was just right. [strongly agree/agree] | 62.5% | 70.3% | 78.4% | 73.5% | 100% | 72.7% | 78.8% |
| Did the event meet your expectations? [yes] | 87.5% | 97.3% | 95.2% | 97.1% | 94.1% | 94.8% | 96.1% |
| Did the event improve your knowledge of the ambulance service? [yes] | 83.3% | 100% | 95.2% | 85.3% | 94.1% | 92.2% | 94.8% |
| Would you like to become involved with our patient and public panel initiative? [yes] | 50% | 37.8% | 33.3% | 29.4% | 29.4% | 35.7% | 40.3% |
| Overall, how satisfied were you with the event? [very satisfied/satisfied] | 87.5% | 97.3% | 92.9% | 94.1% | 94.1% | 89.6% | 88.6% |
Learning and improvements
Following feedback given at the 2023/24 events, we implemented the following changes during this cycle of events:
- To accommodate more questions, we created a second question and answer session: the first taking place before lunch, the second after lunch.
- We included an extra session at the end of the event where attendees could remain behind and talk with staff about their experiences or concerns with our services on a more private, one-to-one basis.
- We invited recruitment colleagues to come along to help with queries about roles with the service.
- We adjusted activity timings as well as start and finish times to give more time for discussion but also allow attendees with children to get away in time for school collection.
- We added a section on how to volunteer and the types of volunteer roles available.
- We obtained name blocks for attendees to write their names on for the tables after out event in Merseyside. Since the name can be easily removed after each event and reused for the next event, this was a more environmentally friendly choice than name badges or an equivalent.
- For 24/25, we will consider other venues as suggested by participants as well as the possibility of a virtual event. Additionally, we will remind our speakers not to use NHS jargon or acronyms and will consider involvement of the other emergency service partners.
Service improvements
- One of our CFRs in Cumbria raised an issue with defibrillator maintenance. We shared their concerns about the availability of defibrillators after usage i.e. quick replacement of pads as well as batteries with the national defibrillator network, the Circuit, which is going to include information about this in their publicity materials. We have featured an article about this in our Your Call magazine which was out in April.
- The Lancashire Council of Mosques has requested cardio pulmonary resuscitation (CPR) training and a visit to Lancashire Mosque schools, we are currently in contact with them to organise this.
- A community group in Cheshire requested information on defibrillator access and whether we offer CPR training, we are currently having discussions to see if we can facilitate this.
- In Lancashire, the Deaf Village suggested there should be a BSL route in for NHS 111 as there is for 999. A colleague from NHS 111 and a member of the Patient Engagement Team visited the Deaf Village to explain to their management all the different ways that deaf patients can access NHS 111.
- In Cheshire, a member of the public asked how an organisation or members of the public can inform us about access details to a property or street. We informed them they can email the Gazetter Team directly. The team will then enter a warning on the property which will be passed to responding ambulance crews in the event of receiving an emergency call.
- Based on low awareness of PTS and NHS 111 services we will continue to produce information materials to keep with this.
- We were asked if we could promote the hospital waiting times app in Cheshire. This has been raised with Cheshire NHS trusts.
- A Lancashire Muslim lady asked us to raise awareness of the need for foot coverings to be worn when entering her home – we will include this information as part of our ongoing cultural awareness activities.
- We have invited to meet with the Jewish community in Manchester and plans are in place for this to take place.
- Volunteering and careers with the ambulance service are of interest to many of our communities so we will look at how these can be incorporated into our events programme.
Next steps
Further to the successful delivery of our five community listening events we will:
- Share this overall summary evaluation report with all attendees and publish the report on our trust website.
- Ensure all feedback themes and learnings are shared with trust service leads.
- Produce an action plan to progress the above actions.
- Produce a proposal and delivery plan for our 2024/25 events programme.
- Update our community contacts database to ensure diversity of representation, in preparation for future events.
- Continue to meet with community groups to update on our services, discuss accessibility issues, and any areas for improvement.
Thank you for attending our listening events and helping us improve services for you and your community. We would love to welcome you back next year with a refreshed format of events. Please spread the word to service users, friends, and family and keep an eye on your inbox for the invite.