Chief Executive’s Statement
I am pleased to introduce the annual Quality Account for 2021/22. This document sets out the work we have done over the past year to improve the quality of our care and keep patients safe, and provides information on key priority areas we are working on in 2022/23.
2021/22 was a year of unprecedented challenge for the NHS and North West Ambulance Service (NWAS), with the continued pressure as a result of Covid-19 being our focus, although not to the exclusion of all else. As we began the year, the country was still very much in the grip of the Covid-19 pandemic, with rising numbers of cases and extremely challenging spring and winter periods. During these periods, we saw the number of 111 and 999 calls rise significantly, putting the service under significant strain.
We have been ensuring that our ‘business as usual’ functions maintained the quality and safety of our services, while striving to provide the best possible response to our patients.
Some of our key achievements during 2021/22 have been:
â– Our continued focus on patient safety.
â– Delivery of quality assurance work aligned to our CQC ratings.
â– Achievements of our trust Right Care strategy goals.
â– The development of a new quality strategy designed by both patients and staff.
â– Maintenance of staff safety (RIDDOR reports) and we are proud of the extensive
work we have done to protect our staff from Covid-19 workplace transition.
2022 will see the introduction of Integrated Care Systems (ICSs), and NWAS has been reviewing its operational and clinical management teams to ensure effective and consistent representation on these. In addition to this, and to support our operational and clinical managers, we have introduced and strengthened additional Partnership and Integration Manager support at ICS and area level. Partnership working across public sector services is vitally important for tackling health inequalities and improving services, and we see ourselves as a key player in this. Our goal is still to develop the safest systems for all patients and staff. This requires every staff member to understand how their role contributes to safety.
Over the last decade, NWAS, like most healthcare organisations, has focused on improving governance, identifying risks, mitigating these through assurance processes, and implementing learning. We are looking forward to sharing our experiences and making improvements from a system perspective.
I have commented before on the resilience, courage, and dedication of our staff, but it is worth saying again that I feel an overriding sense of immense pride in how hard everyone has worked and continues to do so. Without doubt, every single member of staff and our volunteers stepped up during this period to ensure that, despite the situation, we were able to continue to provide the best possible service to our patients. I would like to thank every single staff member and volunteer for their outstanding efforts.
We intend to continue on this trajectory, making all of our services safe, effective, and sustainable for our patients.
Daren Mochrie QAM, MBA, Dip IMC RCSEd, MCPara
Chief Executive Officer
1.1. Statement of Directors’ Responsibilities in Respect of the Quality Account
The directors are required under the Health Act 2009, National Health Service (Quality
Accounts) Regulations 2010 and National Health Service (Quality Account) Amendment
Regulation 2011 to prepare Quality Accounts for each financial year. The Department of
Health has issued guidance on the form and content of annual Quality Accounts (which
incorporate the above legal requirements).
In preparing the Quality Account, directors are required to take steps to satisfy themselves
that:
â– The Quality Account presents a balanced picture of the trust’s performance over the
period covered.
â– The performance information reported in the Quality Account is reliable and accurate.
â– There are proper internal controls over the collection and reporting of the measures
of performance included in the Quality Account, and these controls are subject to
review to confirm that they are working effectively in practice.
â– The data underpinning the measures of performance reported in the Quality Account
is robust and reliable, conforms to specified data quality standards and prescribed
definitions, is subject to appropriate scrutiny and review; and the Quality Account has
been prepared in accordance with Department of Health guidance.
The directors confirm to the best of their knowledge and belief they have complied with the
above requirements in preparing the Quality Account.
By order of the Board
2. Trust Overview
NWAS was established on 1 July 2006 following the merger of the Cumbria, Greater Manchester, Lancashire, and Mersey Regional ambulance trusts. One of the largest ambulance trusts in England, NWAS provides services to a population of around seven million people across a geographical area of approximately 5,400 square miles. The trust employs just over 6,800 staff who operate from over 100 sites across the region and provides services for patients in a combination of rural and urban communities, in coastal resorts, affluent areas, and in some of the most deprived inner-city areas in the country. We also provide services to a significant transient population of tourists, students, and commuters. The North West region is one of the most culturally diverse areas in England, with over 50 different languages spoken by members of the community. Consequently, the trust places considerable emphasis on equality and diversity and public engagement activities to ensure that our services are accessible to all members of the community.
During 2021/22, a focus for NWAS has been the opportunity to further work in partnership and build relationships around the newly forming Integrated Care Systems (ICS) to support the delivery of urgent and emergency care pathways and public/population health agendas.
From 1 July 2022, Integrated Care Systems will become statutory. ICSs bring together
commissioners of NHS services with health and care providers and other partners who work
together to deliver services which meet the needs of specific populations. Each ICS share
four primary goals of;
â– Working together and supporting integration
â– Reducing bureaucracy
â– Enhancing public confidence and accountability
â– Supporting public health, social care, quality, and safety
NWAS areas spans 5 ICSs, these are:
â– Lancashire & South Cumbria Health & Care Partnership
â– Cheshire & Merseyside Health & Care Partnership
â– Greater Manchester Health & Social Care Partnership
â– North East & North Cumbria ICS
â– Joined Up Care Derbyshire
Providing services as a trusted partner across systems, national guidance (Integrated Care Systems Design Framework, June 2021) indicates that NWAS should operate within ‘supra ICS’ arrangements, where multiple ICS NHS bodies will need to work together to develop a shared plan across these systems. The governance arrangements to support this should be co-designed between the related provider and the ICS NHS bodies’ clinical networks or alliances, and, where relevant, NHSE/I regional teams.
We are considered to be a ‘formal partner’ of Lancashire & South Cumbria, Cheshire & Merseyside, and Greater Manchester ICSs, leading to an enhanced relationship within formal governance structures in those areas, namely each Acute Provider Collaborative and area Quality Committees with regional oversight through the Quality Surveillance Group. For North East & North Cumbria and Derbyshire, we are considered a ‘stakeholder,’ a trusted partner who can influence and impact in support of the primary goals and whose activities are impacted by the decisions of the Integrated Care Board. We only provide services to very small populations in North Cumbria and Derbyshire. In these areas, our engagement and governance relationship is at ‘place,’ rather than across the whole ICS, defining the way in which we assure prominence of quality & safety in the local governance architecture. The focus of our partnership and engagement through this statutory change in each area is to ensure we are appropriately represented to maximise the benefits for the system and our communities.
NWAS is engaged in a number of clinical networks, pathway development, and service change processes across the region. Stroke and cardiac improvement programmes align to end-to-end work that spans the patient journey from prevention through to rehab, for example. Nationally sponsored programmes to promote alternative services to emergency departments (virtual ward, urgent community response, same day emergency care, and community diagnostic centres) are all under development regionally, with NWAS as a key partner in their design to support the right care and best experience for patients and communities.
The trust monitors and manages service change using a set of reconfiguration principles defined by NHS England and Improvement (NHSE/I), and works both locally with partners, regionally with commissioners, and more broadly with NHSE/I to ensure visibility and oversight of the many changes, whilst assessing any impacts to NWAS and those programmes of work.
2.1. Trust Vision and Aims
North West Ambulance Service is in the privileged position of touching people’s lives when they need us most. Our core purpose is to save lives, prevent harm, and offer services which optimise the likelihood of outstanding patient outcomes. Every day, our people go the extra mile to live up to these expectations.
NWAS is committed to delivering safe, outstanding care for every patient, treating them with respect and dignity, every time, and building a healthy, inclusive, and engaged workforce. We work in partnership with other services and strive to provide a better service to our population through continuous quality improvement.
To realise this vision, we created our trust strategy and quality strategy, known as the Right Care strategy. Our Right Care strategy outlines a bold commitment from NWAS to go even further to reduce avoidable harm and unwarranted variation, exceeding the expectations of our patients and staff. During 2021/22, significant patient, staff, and public engagement work has taken place to inform the future iteration of the trust and quality strategies, which will be available in summer 2022.
Our values form the foundation of, and drive the whole organisation, ensuring we lead by example and create the right culture and conditions for patients to receive safe and effective care every time. These values can only be achieved if we have the staff in place who share the trust’s values and feel supported to deliver them. We need to ensure that we recruit, develop, and support our staff to feel engaged and proud to work for the trust.
The NWAS values recognise the fundamental importance of inclusion, respect, and striving to deliver our best for patients and our people.
Our vision is to be the best ambulance service in the UK, providing the right care, at the right time, in the right place, every time.
Our priorities are:
â– Urgent and emergency care (integrated care): Increasing service integration
and leading improvements across the healthcare system in the North West.
â– Quality (right care): Delivering appropriate care which is safe, effective and
patient-centred for each individual.
â– Digital: Radically improving how we meet the needs of patients and staff every
time they interact with our digital services.
â– Business and commercial development: Developing skills and capability to
explore business opportunities for current and new viable contracts, services or
products.
â– Workforce: Engaging and empowering our leaders and staff to develop, adapt and
embrace new ways of delivering the right care.
â– Stakeholder relationships: Building and strengthening relationships that enable
us to achieve our vision.
â– Infrastructure: Reviewing our estates and fleet to reflect the needs of the future
service model.
â– Environment: Committing to reduce emissions by embracing new technology
including electric vehicles.
3. Our Services
NHS 111: Delivers 111 services for the North West region and is a major contributor to the delivery of integrated urgent care.
Paramedic Emergency Service (PES) or 999: Includes solo responders, double-crewed ambulances, and volunteer community responders who provide emergency care for 999 and urgent calls for the population of the North West.
Emergency Operation Centre (EOC): Receives and triages 999 calls from members of the public, as well as other emergency services. EOC staff provide advice and dispatch ambulance services to the scene as appropriate. The Clinical Hub (CHUB) is based within the EOC and assesses patients via telephone, providing the most appropriate care based on that assessment, known as Hear and Treat (H&T). This may include dispatching an ambulance (either emergency or urgent care), GP referral, referral to other services, or recommending self-care.
Resilience: Our hazardous area response team (HART) and resilience teams respond to major incidents, fulfilling the trust’s statutory responsibilities as a Category 1 responder under the Civil Contingencies Act 2004.
Patient Transport Services (PTS): Provides essential transport to non-emergency patients in Cumbria, Lancashire, Merseyside, and Greater Manchester who are unable to make their own way to or from hospitals, outpatient clinics, or other treatment centres.
Corporate Services: In addition to providing clinical services to patients, NWAS offers a wide array of specialist, non-clinical corporate services. These teams support staff to deliver the highest possible quality care, be innovative, and respond effectively to patients’ individual needs. Key services include estates and facilities, communications, risk management, digital, vehicle maintenance, finance, and human resources.
Volunteering: NWAS has one of the largest and longest-established Community First Responder (CFR) schemes in England, with 626 active CFRs across all areas of the North West. CFRs are volunteers who live and work in local communities. They are trained and activated by the trust to attend certain critical calls, such as chest pain or cardiac arrest, where time is vital. CFRs provide care until the emergency ambulance arrives. All responders are equipped appropriately with the necessary PPE and regularly review their equipment to meet organizational and national standards.
The Patient Transport volunteer car drivers also play an invaluable role in transporting patients to and from hospital appointments, including renal dialysis, oncology, and routine appointments. The 200 operational volunteers transport patients in their own vehicles while offering a friendly face and a listening ear, helping to put patients at ease, especially those anxious about their appointments.
Volunteers are also involved in our Patient and Public Panel, which has grown significantly to 213 members. A key focus for 2021/22 has been increasing the diversity of the panel to ensure it represents all communities across the North West.
4. Operational Performance
4.1. NHS 111
In 2021/22, NHS 111 continued to experience increased call volumes and a new call profile not previously seen in the service. The call volatility experienced during the early months of the Covid-19 pandemic was replaced by high call volumes, particularly in the mornings on weekdays, with Monday mornings seeing the highest demand.
The recruitment programme during 2021/22 has been extensive, with 241 FTE new frontline staff being recruited and trained between April 2021 and March 2022. Unfortunately, over the past 10 months, there has been a rise in 111 attrition rates, especially in the health advisor role, which has further increased the need to recruit and train new staff. The introduction of a retention premium in the last quarter of the year has led to a reduction in the attrition rate.
Performance Standards
The pressure from increased demand has also created further challenges in performance, particularly for the headline KPI of calls answered in 60 seconds 95% of the time. On average, there were approximately 27,000 more calls offered per month in 2021/22 than in 2020/21.
Performance standards were:
| Calls abandoned | <5% | 2020/21 | 13.67% | 13.12% | 15.04% | 5.90% |
| Calls abandoned | <5% | 2021/22 | 14.21% | 27.61% | 28.07% | 22.54% |
| Calls answered in 60 seconds | 95% | 2020/21 | 64.62% | 62.96% | 57.56% | 70.42% |
| Calls answered in 60 seconds | 95% | 2021/22 | 47.52% | 28.45% | 29.32% | 33.84% |
| Calls warm transferred | 75% | 2020/21 | 21.87% | 19.16% | 18.28% | 6.86% |
| Calls warm transferred | 75% | 2021/22 | 19.23% | 15.08% | 12.54% | 12.16% |
| Call backs within 10 minutes | 75% | 2020/21 | 20.13% | 16.08% | 8.60% | 7.88% |
| Call backs within 10 minutes | 75% | 2021/22 | 5.49% | 4.87% | 4.71% | 6.49% |
During 2021/22 the following improvements were undertaken:
â– New roles: 111 recruited a new role of a Quality and Assurance Officer. This is a
varied role of audit, training support, preceptorship and undertaking non-clinical
advice shifts.
â– 111 SharePoint site; went live in November 2021. Prior to its introduction, 111 relied
very heavily on email to communicate important information with staff. Quality
improvement methodologies were used to make improvements to this process. Now
staff have one central location for all documentation, procedures, educational bulletins and memos. The SharePoint site also gives staff the opportunity to share other important messages e.g. around health & wellbeing, social events or CQC inspections. Staff feedback on the site has been very positive and the number of views has been steadily increasing.
â– 111 Champions: Over the past 12 months the 111 Champion role has become
embedded. The team support staff through celebration days, feedback through the
learning forum, and development forum’s. They not only support all the 111 staff but
also provide feedback to the leadership team.
â– Directory of Services (DoS); task and finish group was created in response to
increased healthcare professional feedback forms relating to use of the DoS. The
group brings together regional and local DoS leads as well as the 111 service
development team and operational staff to make improvements to how services are
navigated.
â– Language Line; provide all translation services to 111. We are currently undertaking
a trial of a new voice recognition system with a small team. The new system will use
voice recognition software to direct the call to the correct interpreter and this should
reduce connection time to an interpreter and improve patient experiences.
â– Testing Text Messaging (SMS): With the support of our commissioners,
executives, NHSE/I and NWAS legal team, 111 have been developing a solution to
enable the service to send end of call care advice via a SMS. This means that subject
to a caller’s agreement they will receive a SMS with a link to a web page. The web
page contains each individual piece of advice that was selected as relevant by the
health advisor. As a result of this we would no longer need to verbalise the advice
for these patients and the patient would be able to refer back to the advice for a
period of 24 hours, after which the link expires. It is anticipated the use of SMS will
enhance patient care, with 24 hour access to the advice and will reduce the length
of each call enabling waiting calls to be answered quicker.
â– Primary Care Networks: Following Covid-19, the 111 team have identified a
significant change in the call profile. In liaison with local and regional commissioners
and Primary Care Networks, work was undertaken to share the information
developed and for commissioners to work with the networks to manage the demand
changes.
4.2. Paramedic Emergency Services
The challenges born out of the Covid-19 pandemic have continued throughout 2021/22. Activity, resources, and acuity have been the primary challenges faced by the trust in delivering Ambulance Response Programme (ARP) standards. Demand has been variable, with peaks observed predominantly in the late spring and early summer, and to a lesser degree, in late autumn and winter. Abstractions of the operational workforce due to sickness and Covid-19-related absence have inhibited the deployment of resources. This has been a continual challenge for the trust, most acutely observed during the winter period. Acuity has also posed a challenge for response, with the trust responding to a higher proportion of Category 1 patients than ever before.
In response to these challenges, the trust has worked with the wider system and other partners to ensure patient safety throughout the year. The trust has utilised Military Aid to Civil Authorities (MACA) for two periods throughout the year, increasing the operational fleet. In addition, the trust has increased the utilisation of private and voluntary services. Working with system partners, a six-point winter plan was developed and delivered to support the system, response standards, and patient safety. The plan focused on increasing 999 call handling capacity, increasing operational capacity, providing additional clinical support, expanding mental health pathways, improving hospital handover times, and retaining the existing operational fleet.
Sector and hospital teams have been working together to improve hospital handover times. To support this work, teams have been involved in quality improvement coaching, testing new ideas using quality improvement methods, and receiving monthly data packs to identify areas for improvement.
Ambulance Response Programme Performance Standards
2021/22 presented a challenging but rewarding year for the Paramedic Emergency Service
(PES) service. Performance standards were:
| Standard | 7 mins | 15 mins | 18mins | 40 mins | 120 mins | 180 mins |
| Q1 | 00:07:55 | 00:13:25 | 00:29:52 | 01:02:45 | 05:13:25 | 11:05:05 |
| Q2 | 00:08:59 | 00:15:18 | 00:54:11 | 01:58:31 | 09:25:59 | 15:55:43 |
| Q3 | 00:09:03 | 00:15:16 | 01:01:07 | 02:17:29 | 09:33:00 | 15:26:52 |
| Q4 | 00:08:41 | 00:14:51 | 00:46:04 | 01:45:54 | 05:54:25 | 11:31:20 |
| Grand Total | 00:08:42 | 00:14:48 | 00:47:39 | 01:47:54 | 07:09:45 | 14:27:14 |
Despite the overall increase in calls during 2021/22, the trust has continued to take less
patients to hospital, delivering safe care closer to home. This has been achieved through
Hear and Treat, See and Treat, signposting of low acuity patients and the introduction of
estimated time of arrival scripts. 37% of emergency contacts into the 999 service were
conveyed and 34% conveyed to an emergency department.
Figure 1 shows the number of 999 calls from April 2018 to March 2022.
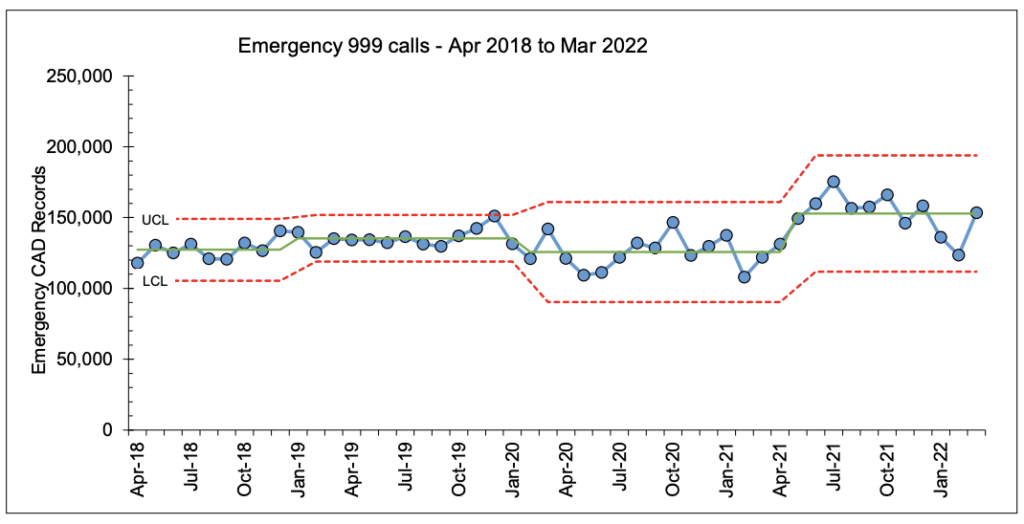
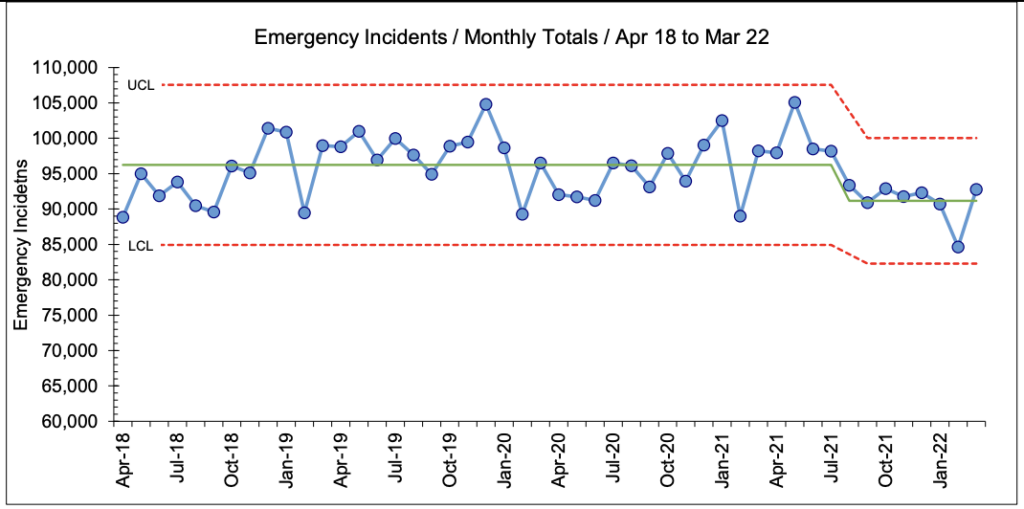
Figure 2 shows the number of ambulances dispatched to the 999 calls from April 2018 to March 2022
The Clinical Hub (CHUB) from Q2 2021/22 has delivered improvements within Hear and Treat. This has been achieved through a change in the triage and dispatch process for Category 3 and 4 incidents. All Category 3 and 4 incidents now receive a clinical review and a decision is made as to whether to dispatch an ambulance or proceed with secondary triage. This approach has increased the overall Hear and Treat rates while ensuring that patients who require an ambulance response receive one.
The CHUB has also increased the number of clinicians through NHS Winter funding. External CAS providers across the Greater Manchester, Cumbria, and Lancashire counties continue to work in partnership with the trust to increase Hear and Treat rates.
The CHUB continues to provide enhanced clinical support across the Emergency Operations Centre (EOC) and the wider Paramedic Emergency Service (PES) team. This support is delivered through clinical guidance to the call handling team via Rotational Specialist Practitioners. The CHUB team also provides crew advice to operational staff, with between 700 and 900 advice calls made per week. Additionally, the team supports the Clinical Coordination Desk (CCD) by triaging long-waiting patients. The CHUB is involved in approximately 40% of all NWAS incidents.
Other NHS providers have also contributed to improving Hear and Treat and See and Treat rates by increasing the accessibility of alternative pathways for NWAS 999 and 111 services. This includes the 2-hour urgent community pathways and Same Day Emergency Care (SDEC) services.
4.3. Emergency Operation Centre
Emergency Calls and Answer Times
The emergency call volume has fluctuated through the year, primarily influenced by the removal of lockdowns and Covid-19 protocols within the community. Throughout the year, call volume has remained high, and the trust has observed record levels of emergency call demand. Emergency calls increased by 28% when compared to the previous financial year.
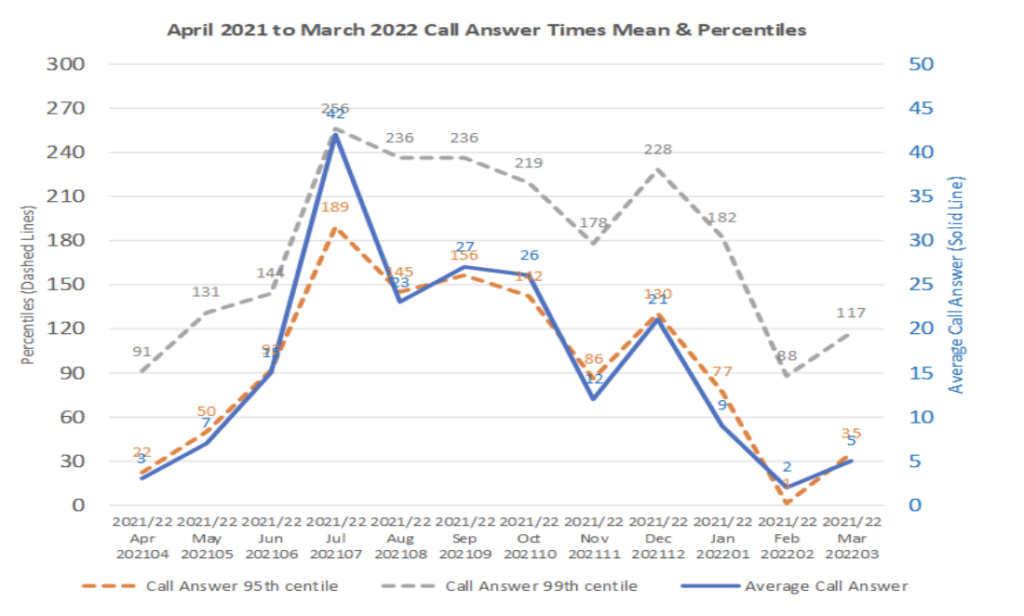
Despite the demand, the trust has continued to deliver high standards of call answering performance. Figure 3 below shows the average time to answer calls against the national standards set. The primary axis shows percentile results (dashed lines), and the secondary axis relates to the mean call answer time (solid line).
Duplicate Calls
On average, NWAS received 1,253 duplicate calls per day during 2021/22, amounting to a total annual volume of 457,433 calls. Duplicate calls are defined as calls received after an initial call, often due to a patient’s condition worsening or to inquire about the estimated time of ambulance arrival. These calls have been a longstanding challenge for NWAS, particularly in response to Category 2 and 3 calls, and represent approximately 30% of the trust’s inbound emergency calls.
Duplicate calls increase the volume of calls that NWAS’s Emergency Operations Centre (EOC) must answer, potentially causing delays in call handling. Over the past year, the issue has worsened across all ambulance trusts. At its peak in July 2021, duplicate calls accounted for approximately 38% of all 999 calls nationally.
To address this issue, both NWAS and BT have implemented measures to reduce duplicate calls. NWAS trialed several initiatives, including calling patients back when incident wait times exceeded the 90th centile response standard. Additionally, NWAS introduced estimated time of arrival (ETA) scripts for Category 2, 3, and 4 patients, with updates provided every four hours to manage patient expectations. Where clinically appropriate, patients were also given the option to self-convey. Concurrently, BT introduced a screening question for 999 callers to determine if the call was solely to inquire about an ETA and not due to a worsening condition.
The ring-back trial did not yield positive results, as it compromised inbound call-handling capacity by redirecting call handlers to make callbacks. As a result, the initiative was discontinued. While ETA scripts have successfully provided patients with more information and led to a significant number opting to self-convey, they have not effectively reduced duplicate calls. Similarly, BT’s screening question has delivered minimal benefits in mitigating the issue.
Less than 1% of total call volume at peak has been deflected by BT, both for NWAS and nationally. Overall analysis, both locally and nationally, indicates that duplicate calls occur and increase as a result of extended response times. Despite efforts to reduce duplicates, there has been limited positive effect.
The trust’s contingency planning arrangements and capabilities assist in providing evidence of compliance with our duties under the Civil Contingencies Act (CCA), 2004, the Health and Social Care Act 2008, Regulations 2010 and the NHS England Emergency Preparedness, Resilience and Response (EPRR) Framework together with other legislation such as the Corporate Manslaughter and Corporate Homicide Act 2007 and the Human Rights Act 1998.
The NHS needs to plan for, and respond to, a wide range of incidents and emergencies that could affect patient care or public health. This manifestations of this could be precipitated by a wide range of triggers from infectious disease as with the current Covid-19 pandemic, transport emergencies, industrial incidents/action, infrastructures failures or terrorist attacks. The Civil Contingencies Act, 2004 requires all NHS organisations and providers of NHS funded care, to demonstrate that they can effectively respond to such incidents whilst maintaining core services.
Under the EPRR arrangements, all NHS trusts which are also designated Category 1 responders under the Civil Contingencies Act, 2004, are required to undertake an annual, self-assessment process to determine the level of compliance of resilience arrangements measured against the NHS England and Improvement (NHSE/I) core standards.
NWAS Emergency Preparedness, Resilience and Response Assessment
- Core Standards: Out of 32 applicable standards, NWAS have self-assessed full compliance with 32 and partial compliance with 0. This represents a compliance figure of 100% and therefore an overall rating of ‘FULL’.
- Interoperable Standards: Out of 163 applicable standards, NWAS have self- assessed full compliance with 145 and partial compliance (including 1 non- compliant) with 17. This represents a compliance figure of 89% and therefore an overall rating of ‘Substantially Compliant’.
The rating of ‘Substantially Compliant’ represents 89-99% compliance with the appropriate core standards with ‘Full’ compliance requiring a 100% rating in each category.
NWAS Emergency Preparedness, Resilience and Response Assessment (111)
- Core Standards: Out of 29 applicable standards, NWAS have self-assessed full compliance with 29 and partial compliance with 0. This represents a compliance figure of 100% and therefore an overall rating of ‘FULL’.
The rating of ‘Full Compliance’ represents 100% compliance with the appropriate core standards.
NHSE/I also require a formal statement of compliance from each trust based on the findings
from the self-assessment process and considering those core standards which necessitate additional attention through the action plan. For 2021/22, the process requires three
separate statements of compliance to be made to indicate performance across EPRR Core Standards (NWAS), EPRR Core Standards (NWAS 111) and Interoperable Standards (NWAS response).
In fulfilling this strategic aim and the requirements of the NHS England Core Standards for EPRR, the thematic work delivered by the resilience team is divided into four specific areas based broadly on the core elements of integrated emergency management:
- Mitigation: Contingency Planning
- Preparedness: Training – Exercising – Learning
- Response: Special Operations
- Recovery: Business Continuity Management
During 2020/21 a dedicated resilience manager for EOC and resilience manager quality improvement were introduced. These roles have strengthened the professionalisation of resilience training and clear auditable evidence around quality improvement has been noted at all levels. Lessons learnt are identified through debriefs, feedback proformas and impromptu or structured reviews of policies and processes either from within the trust or external agencies. The aim is to share best practice, adapt and improve the trust processes as required and enhance the learning culture through the utility of the Resilience team. The dedicated quality improvement manager also attends all areas learning forums with a clear debrief and outlines the learning process.
This year we focussed on the identification of 218 outstanding recommendations from debrief reports and the owner of each action. 101 of these recommendations have been closed, by including them into training but more importantly reviewing those learning outcomes through the continuation of plan do study action methodologies and the debrief from further incidents.
A full rewrite of the trust debrief policy took place, which is a fundamental for any establishment that values learning from situations it has experienced, or when preparing for upcoming events. The policy is designed to provide a process, easy to follow and enabling actions from debriefs to be completed in a timely manner. All data which is gathered using the debrief process can be interrogated to identify trends across all areas, providing the Trust the opportunity to plan and adapt how day to day business is conducted, thereby utilising theses learning opportunities to best effects.
Business Continuity systems have been upgraded with the introduction of an electronic system call ‘Continuity2’. NWAS’s business continuity manager has taken a lead in revamping the winter planning for the trust along with developing a new policy and procedure for the trust’s fuel plan.
Special Operations
Special operations encompass a number of disciplines including:
- Hazardous Area Response Teams (HART)
- Chemical Biological Radiological and Nuclear (CBRNe) response
- Marauding Terrorist Attack (MTA) response
- Special Operations Response Team enhancement programme (SORT)
- Medical Emergency Response Incident Teams (MERIT)
- Command training
- Major incident fleet
- National Inter Agency Liaison Officers (NILOs) and Tactical Advisors
Hazardous Area Response Teams (HART) are comprised of specially recruited personnel who are trained and equipped to provide the ambulance response to high-risk and complex emergency situations. HART teams are based in each of England’s ten NHS ambulance trusts. Working alongside Police and Fire & Rescue Services within what is known as the ‘inner cordon’ (or ‘hot zone’), the job of HART is to triage and treat casualties in such difficult environments.
A significant part of their role is to maintain safe systems of work by constantly training to ensure they are ready to respond to the most complex and hazardous incidents. Annually they are required to maintain competence in the following:
- Swiftwater and flood response
- Safe working at height
- Extended duration breathing apparatus
- High risk confined space
- All terrain vehicle operations
- NXGEN specialist Personal Protective Equipment (PPE)
- High consequence infectious diseases incl. EpiShuttle
- Combined with a full clinical competence framework top paramedic and specialist paramedic standard
Special Operations Response Team (SORT) are comprised of 300 volunteer clinicians from around the trust whose day-to-day role is deployment on ambulances and rapid response vehicles. Trained in chemical, biological, radiological and nuclear (CBRN) response as well as Marauding Terrorist Attack (MTA) response they undergo 7 days training and assessment annually and can be mobilised along with their HART colleagues to terrorist related incidents.
Supporting the specialist response are our Medical Emergency Response Incident Teams (MERIT), comprised of up to 40 experienced senior doctors who have had additional training in major and complex incidents and provide medico legal advice to the command cadres and responding clinicians. Undertaking regular exercises and recertifying annually MERIT are an integral partner in our effective incident response.
A key responsibility of the special operations team is the continued training and support given in relation to effective command of NHS assets at major and complex incidents. Coordinating a programme of national training courses to ensure appropriate succession planning at all 3 command levels those of Strategic Tactical and Operational command they also provide bi-annual in-house training opportunities for commanders to maintain their continued professional development in line with national occupational standards.
Aligned to NWAS’s command cadres is our Tactical Advisor / National Interagency Liaison Officer capability. Drawn from resilience and special operations managers the capability are nationally qualified to provide advice both internally to NWAS commanders and externally to partner agencies on the specialist capabilities of all emergency services and specialist military assets.
4.5. Patient Transport Services
Much of 2021/22 was influenced by the ongoing Covid-19 pandemic. For Patient Transport Service (PTS) this has meant transporting overall lower volumes of patient journeys (activity) than contracted. Activity during the financial year (April 21 – March 2022) was 24% below contract baseline, whilst the contract year (July 2021 – March 2022) was 23% below baseline as shown in the table below.
Performance Standards
2021/22 presented a challenging but rewarding year for the PTS service. Performance standards were:
| NORTH WEST AMBULANCE PTS ACTIVITY SUMMARY | |||||||||
Contract | Annual Baseline | Financial Year 01/04/2021 – 31/03/2022 | Contract Year 01/07/2021 – 31/03/2022 | ||||||
Baseline | Activity | Activity Variance | Activity Variance % | Baseline | Activity | Activity Variance | Activity Variance % | ||
| Cumbria | 168,290 | 168,290 | 111,081 | (57,209) | (34%) | 126,218 | 84,236 | (41,982) | (33%) |
| Greater Manchester | 526,588 | 526,588 | 440,617 | (85,971) | (16%) | 394,941 | 336,857 | (58,084) | (15%) |
| Lancashire | 589,181 | 589,181 | 396,330 | (192,851) | (33%) | 441,886 | 300,936 | (140,950) | (32%) |
| Merseyside | 300,123 | 300,123 | 260,957 | (39,166) | (13%) | 225,092 | 197,153 | (27,939) | (12%) |
| Grand Total | 1,584,182 | 1,584,182 | 1,208,985 | (375,197) | (24%) | 1,188,137 | 919,182 | (268,955) | (23%) |
Although activity volumes are below baseline levels, the way in which PTS is able to utilise its resources has changed significantly. As a result of social distancing measures only a maximum of one patient can travel in a taxi or volunteer car at a time, and a maximum of two patients can travel on an ambulance where a distance of 1 metre plus can be accommodated. This continues to cause challenges in meeting demand which is subsequently met by increased use of private ambulance provision, as care systems implement their outpatient restoration plans.
Throughout the trust’s response to Covid-19, PTS has continued to adapt to the changing demands placed on the service in terms of activity fluctuations and other associated challenges but has maintained its support of the paramedic emergency service (PES) via the supply of staff and fleet resources in the form of PES assistants and blue light drivers. As a result of these initiatives many PTS staff have enjoyed career progression and have now taken up substantive posts within PES. Although these initiatives were clearly positive for the trust, and our staff, the temporary nature of the arrangements has put pressure on the service due to the level of and speed with which, vacancies were created.
Work will continue with regards to the use, management and oversight of private ambulance providers into the ensuing year. The support shown by our private ambulance providers partners has been critical in our ability to safely deliver services throughout the year. We are also supported by a cadre of approximately 200 volunteer car drivers.
During 2021/22 the following improvements were undertaken:
- Safer discharge; guidance produced which has been distributed to NWAS and third-party ambulance providers.
- Training: Changes to the classroom mandatory training to address areas identified for improvement during the forum meetings.
- Patient safety: Process agreed to better manage skin tears for patients with fragile skin.
- Bulletin; produced outlining good practice when discharging immobile patients.
- Communications issued to third party providers regarding Personal Protective Equipment (PPE) and Infection Prevention & Control (IPC) requirements.
System developments; made to allow trend analysis of third-party provider complaints.
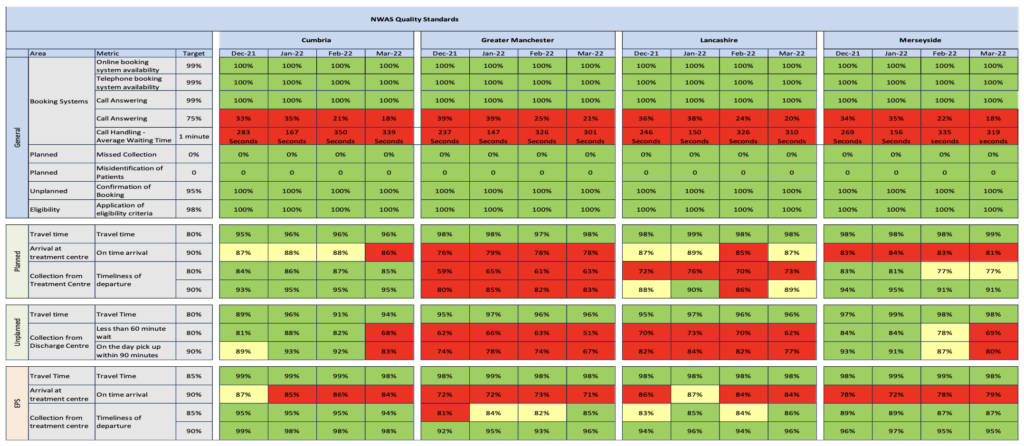
For the purpose of oversight, the table below shows PTS performance from December 2021 to March 2022.
4.6. Community First Responders
Community First Responders are volunteers who are trained and activated by the trust to attend certain calls, such as chest pain or cardiac arrest, where time to respond is critical and can make the difference between life and death. The responder provides care and support to the patient until the arrival of an emergency ambulance. Quite often, the role of a responder is one of reassurance and, in some instances, for example when a patient has chest pains, simply giving oxygen can make a big difference. However, in extreme cases, the CFR can perform cardio-pulmonary resuscitation (CPR) or use a defibrillator to restart the heart. Chances of survival decrease by 10% with each minute that a person’s heart has stopped beating, and CFR availability in the local area can result in a quick response to ensure that treatment is started as early as possible. Survival rates can be as high as 80% if an automated external defibrillator (AED) is used within the first 4 minutes of the cardiac arrest occurring.
We have continued to support and proactively engage with communities, organisations, and individuals with the placement of AEDs in their communities. These life saving devices are a vital part in increasing the chances of survival form a person suffering an out of hospital cardiac arrest. Within NWAS, we have over 2956 community public access defibrillators, which are devices that are available 24 hours a day, 7 days a week. These are placed in locked, heated and coded boxes and members of the public can be directed to them in an emergency and instructed how to use via the emergency call taker in an emergency. In addition to these devices there are a further 7810 defibrillators registered with NWAS that are located in numerous buildings and again accessible if required. These buildings range from leisure centres, shopping centres, supermarkets, healthcare setting, schools etc.
In this past year, we have worked closely with the British Heart Foundation to implement a new system to allow the public to register their AED’s on a national system called ‘The CIRCUIT’. This allows for a central place for the public to register and then allow the ambulance service to send someone to the AED in an emergency. The system is fully integrated to allow us to know exact locations of AED’s and then support communities in their time of need.
During 2021/22, our volunteers have provided unwavering support to communities and added resilience to our service. Over 110,000 hours’ worth of volunteer support have been given to communities and the trust responding to emergency calls by this group of volunteers for the period of 2021/22. During the past year, we have continued the challenges brought upon us by the pandemic, we have faced challenges never experienced before and the support that has been given by our volunteers enabled NWAS operational crews to continue to deliver the best care to the people of the North West.
In addition to this vital support many other tasks were supported by our volunteers, below outlines a snapshot of these:
- Manned welfare vehicles; located at ED’s to allow crews access to refreshments.
- Delivery of PPE and medical stores; to the 100 stations throughout the North West.
- Enhanced level of knowledge to responders; to allow them to attend low acuity emergencies and have clinical support available to see if an emergency ambulance was required for the patient.
- Assisted in the LAMP Covid-19 testing; processes across a number of NWAS sights.
Provided marshalling; roles at the NWAS vaccination hub.
The pandemic brought an increase in emergency calls and the additional support from our enhanced community first responders. This group of responders continued to work on emergency ambulances with core staff in a bank contract capacity. This increased the availability of ambulances for emergencies.
Membership of a Community First Responder scheme can be incredibly rewarding, and volunteers could be involved in saving someone’s life. Anyone who lives or works in the North West can get involved with their local CFR scheme, by either becoming a First Responder or helping with other vital tasks such as fund-raising, support or administration. Volunteers do not need previous first aid experience to join their local group, as full training will be provided. Further details on Community First Responder schemes are available at
5. Our Quality Strategy
5.1. Safety
Our goal is to develop the safest system for all patients and staff. This requires every staff member to understand their role and how it contributes to safety. Each month, NWAS colleagues report more than 1,350 adverse incidents. The ambulance service is fraught with complexity and the risks of error have been well documented. Over the last decade NWAS, like most healthcare organisations, has focused on improving governance, identifying risks, mitigating these through assurance processes and implementing learning. Safety has become core business and our strategy seeks to take these foundations to the next level focusing on safety improvement.
During 2021/22 NWAS has invested in new roles to support maternity and mental health
pathways and care quality in these areas. The work programmes led by these roles are detailed in section 7.1. of this document.
5.2. Effectiveness
Our goal is to provide clinically effective service using research evidence and agreed professional standards to improve clinical practice and service delivery through clinical audit, review, learning and improvement. In our Right Care strategy, we focus on priority areas to improve the reliability of evidence-based care standards of:
- Cardiac arrest
- Stroke
- Sepsis
- Vulnerable patients (including frailty, mental health).
- Preventing harm to patients who wait for our services (deterioration/self-harm)
This is still a focus of our new quality strategy too, which will be published in summer 2022
5.3. Patient Experience
Our third commitment to our 999, 111 and PTS patients is to listen to their feedback, work
with them to re-design care and provide personalised care, every time. NWAS interacts with
the North West population through several public engagement channels. This work is a
Page | 21 focus for our communications and engagement team and is led by the Director of Strategy
and Planning.
5.4. Pillars of Quality
Our fourth commitment is to ensure that underlying processes of care, essential to delivering
high quality care, are continuously improved. Importantly these ‘pillars of quality’ run through
our organisation and there is no department or service line immune from ensuring that we
deliver the highest standards of care under these domains. The six domains are:
â– Complaints and Compliments
â– Incident reporting (including serious incidents)
â– Safeguarding
â– Health, safety and security
â– Infection prevention and control (IPC)
â– Medicines management
Our strategy signals our intention to progress these six pillars of quality to previously
unprecedented levels of performance.
6. Our Improvement Approach
6.1. Method
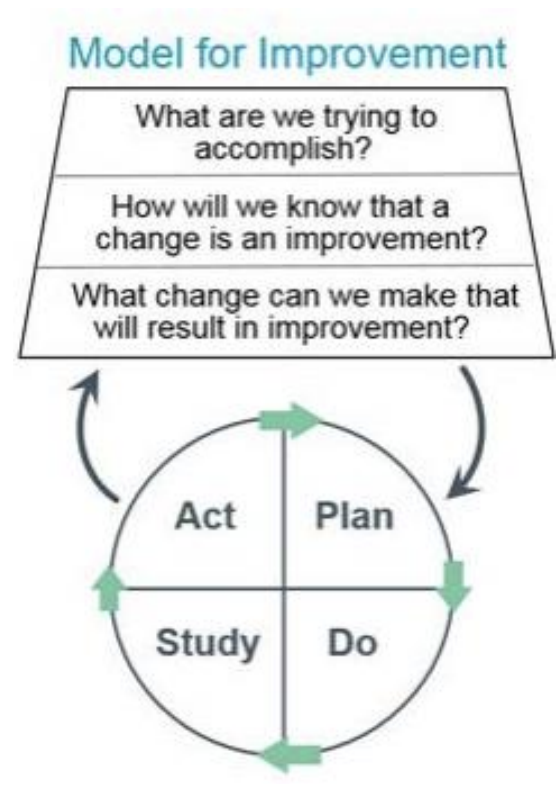
Our approach to improvement is grounded in the theoretical models of Deming, Juran and Shewhart. We use the Model for Improvement developed by the Institute for Healthcare Improvement. This is a method which asks teams to address three key questions and use Plan, Do, Study Act cycles to instigate small tests of change which build learning about how systems are working. This methodology is deceptively simple but has shown proven benefit across a range of industries. The Model for Improvement requires teams to focus on setting an explicit, measurable, time limited goal. It seeks agreement on a set of measures which will be tracked frequently (often daily or weekly) and asks teams to organise their thinking to focus on the specific changes which will make the most significant impact on the goals. Organising these thoughts into a driver diagram or logic model helps teams to agree on leadership responsibilities.
6.2. Measurement and Intelligence
We continue to commit to building a system of real time quality measurement and feedback to the service which can be used for performance, quality surveillance and improvement. We are building measures for key programmes of work and providing real time data back to the service. In addition, we have now rolled out Power BI which provides real time data through several self-access dashboards. Regular reports are now shared from SafeCheck, our compliance platform, with quality and safety data triangulated in a quality compliance scorecard. The monthly integrated performance report provides assurance to the board each month on a range of indicators, including quality, effectiveness and patient experience.
6.3. Skills Training
We continue to prioritise the building of improvement skills in individuals and teams, focusing on patient care priority areas. We continue to build our quality improvement network and design forums to systematically develop the talent and ideas of our workforce using techniques such as leadership development, patient stories, driver diagrams, process mapping, measurement of variation (statistical process control) and the model for improvement. Small tests of change, which build cyclically, are tested, and used throughout the organisation.
During 2021/22 10 Quality Improvement (QI) Network sessions have been delivered and the network membership has increased to 147 members. Staff feedback has shown:
- 4.78/5 is the average rating of the QI Network sessions.
- 4.22/5 is the average rating of attendees in agreement that there was a sharing and spreading of ideas.
- 4.22/5 is the average rating of attendees in agreement that they were developing QI capability.
Topics covered in the QI Network include:
- QI methods: Aim statements, driver diagrams, measurement for improvement, PDSA cycles, visual management and 6S.
- Theory: NHS Change Model, Human factors and defining quality.
- Engagement: Storytelling and stakeholder engagement models.
- Data: Using public health data to identify improvements areas.
- QI and project documentation; and coaching support.
Case studies have included:
- Learning from patient safety incidents.
- East Lancashire social prescribing project.
- Using PDSA cycles to test the 4AT (delirium) tool in South Manchester.
- NWAS learning from Covid-19 and how we responded to the pandemic.
- Implementing digital communication solutions to share 111 pathways updates with staff.
- Improving cardiac arrest outcomes for patients using public health data.
- Burnley station 6S, equipment and supplies improvement project
- Hospital handover action cards and improvements at Warrington hospital emergency department.
During 2021/22 staff have also been offered the opportunity to enrol on 90-minute QI virtual sessions covering the following topics:
- An introduction to Quality Improvement
- Starting your test of change
- Measurement for improvement
- Creating a change culture
Quality Improvement training delivery has continued virtually to make it more accessible for shift working, organisational geographic spread and new ways of working since the pandemic to reduce infection spreading risks during the Covid-19 waves.
Our Digital Design Forum has continued to provide a space for staff to bring ideas and / or problems and work with the digital teams to use improvement methods to test digital solutions. Ideas are presented weekly and around 30% have gone forward to full implementation following testing. Products and solutions tested in 2021/22 have included:
- Communication and knowledge management platforms for multiple teams.
- Digitising key workforce processes such as timesheets.
- Staff led developments for our electronic patient record.
- Ways to link up our systems including a single patient index for patient flags.
- Access to British Sign Language interpreters from on scene.
- Station wallboard solutions.
6.4. Quality Assurance Visits
We continue to focus on the design and testing of a standardised process for quality assurance. Importantly the quality visits reward those teams who perform well with an acknowledged performance status and identify those areas requiring further support and more frequent review. The implementation of this system of visits is critical to ensuring management oversight and corporate assurance on key standards.
6.5. Evaluation
The evaluation function was newly established in March 2021 to support continued learning about ‘what works, and why?’ following change, redesign and quality improvement work. During 2021/22, evaluations have been undertaken of trust’s emergency department contract cleaning service, the Smart Sites pilot programme, the Every Minute Matters, hospital handover collaborative and the SafeCheck platform. Learning from the evaluation reports have been shared internally with a plan to publish some of the learning externally in 2022/23. Some of the evaluation learning has informed:
- The roll out of Smart sites using digital technology over summer 2022
- How SafeCheck with be modified to support internal Quality Assurance Visit (QAV’s) and be enhanced to have more functionality
- The development of hospital handover learning case studies
A key element of the function has also been to build evaluation capability across the organisation, with evaluation training and coaching being delivered to staff across a number of functions in NWAS.
7. Our Improvements 2021/22
7.1. Safety
Safety
The safety of our patients and staff has continued to be a priority for NWAS in 2021/22 and assurance of our ongoing commitment to be the safest we can be, is overseen through a refreshed governance structure including the Health, Safety and Security sub-committee, Patient Safety sub-committee and Clinical Effectiveness sub-committees. Each sub- committee provides a chairs assurance report to the Quality and Performance committee that the trust is delivering the required standards and improvement, and reporting any risks identified. In 2021/22 each sub-committee has been assessed against its terms of reference to understand what governance changes were required to meet the delivery of work programmes.
Safety Culture
At NWAS, we encourage all our staff to report risks, near misses and incidents, and ensure we can learn to prevent future harm. Whilst there is still work to do in terms of developing our safety culture, we are pleased to see improvement in several of the questions relating to safety and speaking up from 2021/22 in the NHS Staff Survey:
- Would feel secure raising concern about unsafe clinical practice (72% in 2021/22 from 68% in 2020/21).
- Would feel confident that organisation would address concerns about unsafe clinical practice (55% in 2021/22 from 53% in 2020/21).
- Feel safe to speak up about anything that concerns me in the organisation (56% in 2021/22 from 59% in 2020/21).
- Feel organisation would address any concerns I raised (44%). This is the first year that this question has been included therefore no comparator.
Work has been undertaken in 2021/22 to ensure that our staff are able to see that incidents reported have been robustly investigated, and that learning has taken place through the building of our Datix Cloud IQ reporting system. There has also been significant work to embed ‘Just Culture’ principles to ensure staff who may have been involved in an incident are treated fairly with maximum opportunity for learning across the organisation, and awareness raising for staff on Duty of Candour to ensure that openness and transparency is embedded through all levels of our organisation.
In response to learning identified from incidents occurring at NWAS, and safety intelligence from medical alerts, national reports and other trusts, action and improvement plans are developed with oversight from internal operational level 3 managers meetings, area learning forums, sub-committees and subject specialist such as the patient safety team or medicines management team. In 2021/22 the organisation has built a number of data dashboards which we will develop further to enable us to predict where safety risks may be and mitigate before incidents occur.
Safety Skills
Safety is improved through education and training and in 2021/22 we have commenced rollout of both level 1 and level 2 of the patient safety syllabus. The syllabus incorporates five domains:
- Systems approach to patient safety
- Learning from incidents
- Human factors, human performance, and safety management
- Creating safe systems
- Being sure about safety
- This will continue to be rolled out across the organisation in 2022/23 according to role. We have also delivered several bespoke training sessions on incident investigation across the organisation, which encompasses just culture to ensure that staff are treated fairly, feel safe to report incidents, and we can learn when incidents occur. The patient safety team have also undertaken training delivered by the Healthcare Safety Investigation Branch (HSIB) to ensure that we can improve patient safety investigations and learning thus preventing future harm.
- The above is in addition to the clinical training we provide to our staff where we highlight safety risks, for example in 2021/22 there have been several training sessions undertaken whereby staff have been able to undertake obstetric emergency simulation with training delivered by the NWAS consultant midwife. This role is very innovative in the ambulance sector.
- The trust also now employs a full time patient safety specialist who will continue to develop programmes of work to improve safety across the organisation, and at system level with our healthcare partners. This work programme is aligned to the national NHS Patient Safety Strategy and implementation of the new Patient Safety Incident Reporting Framework (PSIRF) outlining how providers should respond to patient safety incidents.
- Safety by Design
- We have continued to use digital solutions aligned to process improvement to design safety into our processes. This has included roll out of SafeCheck which enables real time recording and management of safety checks and SMART stations which has included several new technologies such as for equipment tracking and controlled drugs keys which increase security whilst providing timely access to controlled drugs.
- Safety in Emergency Operations Centres (EOC) and Clinical HUB (CHUB)
- The team have continued to deliver service improvement, enhance patient safety and respond to patients effectively. The primary achievements for this year are as follows:
- Introduction of modified virtual Covid-19 wards.
- Introduce several quality and compliance checks (call passing, ineffective breathing, subsequent calls, and Protocol 36).
- Introduction of call handling team leader role.
- Introduction of signposting for low acuity patients.
- Changes to the EIDS tool.
- Introduction of SharePoint to enhance staff engagement and communication. Accessed by call-handers and dispatch roles to promote shared awareness, learning and fast dissemination of information. This has allowed for more timely, accurate and high-quality briefing of staff when rapid procedural changes are required.
- Implementation of BBR rosters.
- Improvement to patient safety including; dispatch best practice programme, patient safety huddles, improved incident reporting and enhanced learning culture.
- Introduction of the Clinical Coordination Desk (CCD) to manage risk within the long waits.
- Launched new interactive reporting wallboards.
- Introduction of the Complex Incident HUB
- New process for the management of Category 3 and Category 4 patients which involves validation of lower acuity incidents via clinical hub, utilising senior clinicians to manage lower acuity patients in a more effective manner, has noted a significant increase in Hear and Treat.
- Delivery of the Unified Communications programme.
- Launch of iPads within EOC.
- Delivery of Phase one of NHS Pathways.
Learning from the Ockenden Report and maternity provisions
NWAS currently provides both telephone and face to face maternity care by a range of ambulance staff including paramedics, and non-registered ambulance staff, with the capability to include the NHS 111 service within its portfolio. Maternity patients and new- borns remain a key patient priority group within NWAS, highlighting the need for a clear approach to addressing current improvement and quality efforts relating to prehospital maternity and new-born care. Reducing unwarranted variation in experience or outcome is a focus for us as a trust. During 2021/22 NWAS appointed a new consultant midwife role to act as a professional point of contact for the maternity services across the Northwest. This role is also a conduit for the regional maternity team in ensuring that risk and governance are escalated to the respective trusts, as well as where a maternity unit has concerns with the delivery of pre-hospital care delivered by NWAS.
The focus for this area of work during 2021/22 has been:
- Incident reporting: Our trust incident reporting platform now supports maternity reporting and has the ability to report incident themes. During 2022/23 the implementation of the Datix IQ platform will support the development of a maternity incident dashboard allowing deeper analysis.
- Patient safety: Guided by national and local reports, NWAS acknowledges the drive for equality and equity in maternity care amongst pregnant patients. The Ockenden report and the MBRRACE report findings are being reviewed against current practice, with a focus on racial disparities amongst pregnant patients across the Northwest of England. NWAS is addressing the immediate and essential actions from the Ockenden report in the context of prehospital maternity care.
- Training and education: A recent service review within the organisation identified and explored staff needs relating to training and education focused on attending and managing maternity related incidents in the pre-hospital setting (Heys et al., 2022). Recommendations from the review have guided the organisation in terms of investment, working closely with the local maternity systems and Health Education England Northwest, investment has secured the pre-hospital PROMPT training package with next steps supporting scale and delivery. To date 60 advanced paramedics and senior paramedic team leaders have attended the pre-hospital PROMPT training. The pilot training area have been in Greater Manchester and South Cumbria and Lancs. The training is being evaluated and assessed for impact.
Mental Health
The NHS Long Term Plan (2019) recognised the significant role that ambulance trusts play in responding to mental health calls, supporting people in mental health crisis, and providing and transporting patients to a safe and appropriate place to receive the care and treatment required. NWAS provides telephone triage and assessment and face to face assessment for people ringing 999 with a mental health need/in a self-defined mental health crisis and telephone triage and advice/signposting via 111 for patients ringing with a mental health related need.
In 2021/22 approximately 8% of all 999 calls to NWAS were in relation to mental health. The year 2021/22 has seen a 5% rise in mental health related 999 calls and a 2% increase in mental health related face to face incidents than the preceding year.
| Year | Emergency Incidents | Face to face incidents |
| 2020 – 2021 | 82,279 | 66,795 |
| 2021 – 2022 | 86,537 | 68, 303 |
| Annual activity comparison | 5% increase | 2% increase |
In recognition of the increasing mental health related calls, the role NWAS must play in supporting people in mental health crisis whilst ensuring a timely response and promoting patient safety several initiatives and developments have been implemented in NWAS and with Integrated Care System (ICS) partners, examples of these are highlighted below:
- Proactive mental wellbeing: There has been significant collaborative work between the people and quality teams to enhance the mental health support offer to staff. Mental health and suicide prevention/post-vention toolkits have been launched to support managers to engage with their staff proactively around their mental health. Since their launch both toolkits have been shared with other organisations to adopt locally. Proactive mental wellbeing calls are being rolled out initially across out contact centres to identify the need for supportive interventions and ‘Beat the Burnout’ sessions have been running to provide holistic support for lifestyle changes. The teams are also working jointly to embed the Association of Ambulance Chief Executives (AACE) mental health continuum across the organisation to further challenge stigmas, support wellbeing conversations and enable effective signposting. In March 2022 the NWAS mental health team won a Cheshire and Merseyside Nursing award for the work they had done in promoting staff wellbeing.
- Integrated care: NWAS presence at regional and ICS mental health related meetings thereby ensuring a voice at the table.
- System working: Development of a regional joint protocol between the Police and NWAS regarding the opening and closing of call logs (in final draft) to ensure ongoing communication where both parties are involved in an incident.
- Implementation of the National Record Locators (NRLs); in the NWAS EOC computers, to enable clinical hub senior clinicians to access mental health crisis plans for patients known to services (If mental health trust have signed up to the system).
- Zero suicide: NWAS are currently working with Zero Suicide Alliance and Mersey Care Trust on ‘ZSA share document’, which provides examples to support clinical teams when it is appropriate to share information on suicidal patients.
- Promotion of services: Working with the NWAS communication team to regularly promote the public mental health crisis line numbers via social media, thereby directing individuals with a mental health need/in mental health crisis to the right professional in a timely manner.
In addition to the above over the last 12 months extensive system partnership working has been undertaken to develop pathways for patients in mental health crisis who ring 999, to increase the numbers of patients managed via Hear and Treat, to reduce long waits and to promote patient safety. Examples of the work developed include:
- Directory of Service: A review and update of services on the Directory of Services (DOS) and ambulance improved pathways on service finder to ensure effective use of commissioned resources. This has included working closely with mental health trusts and commissioners to gain access to professional lines so NWAS clinicians can gain advice and guidance from mental health professionals regarding mental health incidents.
- Public sector services working together: In October 2021 within the Greater Manchester (GM) footprint mental health huddles were commenced to help provide timely mental health care for people in crisis and reduce long waits. Huddles involve NWAS, GM Police and senior practitioners from the crisis helplines in GM Mental Health and Pennine Care trusts. They are designed to identify those people who can be appropriately diverted to services that can meet their needs outside of the urgent and emergency care system. Outcomes include clinical information sharing to inform shared multidisciplinary, risk-based decision making, most calls accepted by mental health providers are either supported by the helplines and closed or signposted/referred into other services, reduction in mental health calls waiting in NWAS stack and a reduction in ambulance response where an alternative can better meet the person’s needs.
- A review of GM clinical assessment service (CAS); acceptance codes so the service can accept an increased number of mental health related incidents.
- EOC: Mental Health Clinicians from Manchester have spent time at EOC in Parkway Manchester. Working with NWAS clinicians and advanced practitioners they have been able to support the closure of calls through referrals into mental health services and information sharing.
- The mental health advice line; situated in Broughton EOC and is staffed by mental health clinicians from Lancashire and South Cumbria Foundation Trust is an established model in NWAS.
- Heath Education England Mental Health Transformation project: Two educational transformation specialists have been seconded to NWAS until December 2022. The project comprises of two phases. Phase 1 is the new entrant mental health induction programme for new ambulance staff across all ambulance trusts and phase 2 is the development of mental health related training material and the identification of future statutory/mandatory requirement for mental health training across ambulance trusts. The project is overseen by an expert reference group and phase 1 is due for completion in early summer 2022.
- Learning disability and autism: Following NWAS successful application to NHS England North Regions Learning Disability and Autism Long Term Planning Bid monies were awarded in April 2021 for optimising ambulance services for patients with learning disability and autism. NWAS aim is to develop and implement a comprehensive and collaborative learning disability and autism strategy that will encompass support for patients across the whole life span, including children and young people, adults and older adults. During the reporting year 21/22 we recruited to a seconded post of 12 months our first LD & A practitioner. We have worked in joint partnership with LD & A Providers, patients, carers and their families to host a series of focus groups in order to identify good practice in NWAS and to identify any gaps to form the strategy. The strategy is in draft form and will be formally launched Summer 2022.
The trust is committed to an open and honest culture, maintaining high standards of patient care, continuously striving to act honesty and with integrity in its approach to management systems, processes, responsibility as an employer and protecting the people within the communities that it serves from harm.
Freedom to speak up (FTSU) has continued to be embedded within the trust during 2021/22 through the work of the Freedom to Speak up guardians and 10 local Freedom to Speak Up champions. The FTSU champions are from both clinical and non-clinical services, geographically dispersed and diverse in terms of demographics, background, and experience and provide staff and volunteers advice and a point of contact to approach to raise a concern.
The trust has an implemented FTSU policy which is undergoing scheduled review during Q1 of 2022/23. Our board receives quarterly assurance reports and an annual report highlights areas of concern and mitigating actions.
Details of ways for staff and volunteers to speak up are provided in detail below.
Ways to Speak Up
Staff can, and are encouraged to raise concerns about individual employment rights or personal treatment (e.g. bullying and harassment) under the appropriate trust policy. Where an individual feels unable to do this, they can contact the trust’s FTSU champions or guardians, who will provide independent and impartial advice regarding the application and procedure associated with raising a concern at work.
The trust has a FTSU policy to protect individuals if they have a reasonable suspicion that malpractice is occurring, has occurred or is likely to occur and it is in the public interest. In the spirit of FTSU, the policy aims to support staff that may wish to speak out about any concern, provides assurance that they will be listened to and their concern will be acted upon. Under the FTSU policy, staff can raise a concern about risk, malpractice or wrongdoing that they think is harming the service we deliver.
The trust’s FTSU guardians are responsible for ensuring that individuals receive appropriate feedback on how issues they speak up about are investigated and where appropriate, conclusion of any such investigation.
There are various ways staff can speak up including a face to face or virtual setting or written format. Issues or concerns can also be raised anonymously or by a named individual, methods include:
- Letter to the Chief Executive Officer (CEO)
- Via trade union representation
- Via members of the People directorate (human resources)
- Speaking to their line manager or a senior manager
- Logging a new incident via Datix IQ
- A member of staff may disclose their concern to occupational health but may have not informed their line manager.
Information relating to FTSU sits on the trust’s intranet (Green room) and includes information on the FTSU guardians and champions, their contact details and how to raise a concern.
FTSU activity 2021/22
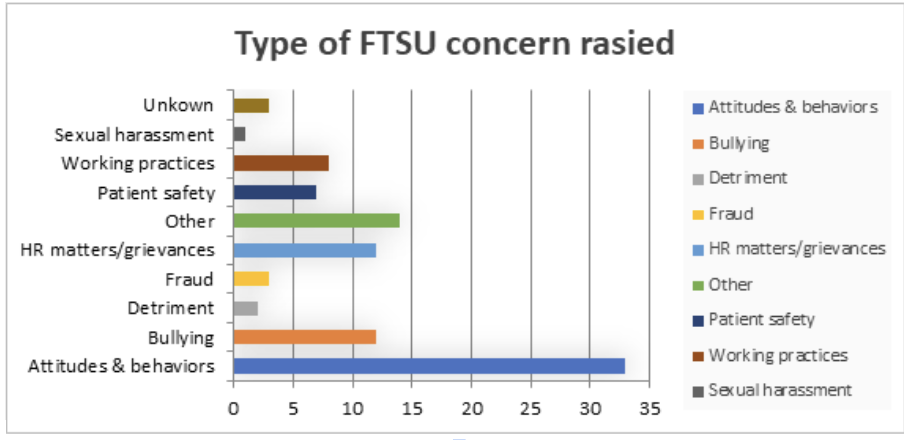
During 2021/22, 98 concerns were raised, a significant decrease (57%) on the previous reporting period (2020/21) when 228 cases were raised. The key themes that emerged were attitudes and behaviours, human resource matters/grievances, bullying and patient safety. Breakdown of the type of concerns for 2021/22 are provided below in Figure 5.
Learning from FTSU
The Executive Director for Corporate Affairs was the executive lead for FTSU during the reporting period with a Non-Executive Director for Freedom to Speak Up who oversees the process. It was agreed that the executive lead would transition to the Medical Director in 2022/23. The change was part of the annual Executive portfolio planning where a stock check was taken to determine what would be the best arrangements going forward for FTSU. Taking into consideration the findings in the Francis Report, which showed unacceptable levels of patient care due to staff cultures deterred from raising concerns, it was determined that FTSU would be ideally placed under the Medical Director with enhanced FTSU guardian support to him but continuing with the strong links already in place between the FTSU team, Non-Executive Director lead and Director of People.
Regular meetings take place between the FTSU guardians and Chief Executive Officer to discuss key themes which are then shared with the wider Executive Leadership committee and relevant board members to consider any risks and further actions for the trust.
During 2021/22 we have made improvements to our FTSU processes and awareness within the trust including:
- Reviewing the FTSU raising concerns policy (final stages of approval).
- Investment in FTSU to further embed into trust with appointment the FTSU lead guardian during Q1 2022/23.
- Oversight and support from consultant paramedic and advance paramedic guardians who have completed FTSU guardian training.
- Strengthening of arrangements given the geographical nature of NWAS and need for resilience and leave cover by having three trained guardians to be more representative of models in the sector.
- Further investment has been made in administration officer support for FTSU and work is currently being scoped to develop the new DATIX Cloud IQ to further enhance reporting and analytical capabilities.
- Regular communications updates across various communication channels.
- Monthly meetings held between the FTSU guardians; Chief Executive, FTSU Executive Lead and the Director of People to provide oversight that the trust’s systems and processes for speaking up are working effectively
- Six weekly meeting with the Head of Service EOC to review open FTSU cases relating to this function.
- Concerns raised around patient safety shared with the Executive Director of Operations and Medical Director to give an overview of the types of concerns,enabling directors to monitor and address common themes identified across their directorates, take ownership and share and embed any learning from them.
- All concerns raised are directed to the executive lead for the directorate the concern relates to, actions are put in place to address these concerns which are audited to ensure they are being taken seriously. Some concerns are escalated to more than one person as the concerns may include more than one category or area of concern.
The trust has worked throughout 2021/22 on positive developments to a healthy speaking up culture. Highlights of this work include:
- Various activities including attendance of FTSU guardians at staff forums, networks, policy groups and senior manager team meetings to encourage and promote FTSU at NWAS.
- Cascade learning from FTSU concerns that have led to improved practices across the trust.
- Identify trends and triangulating data to create insight into safety culture.
- Promoting the outputs and learning from the organisational wellbeing audit run by an independent consultancy who specialise in organisational culture and development (Zeal Solutions).
- Promote the ‘Treat Me Right’ campaign and the relaunch of the trust values promoting dignity and respect in the workplace.
- Raise awareness of FTSU during ‘Speak Up Month’.
- Support the ‘Be Think Do’ leadership programme.
- Support staff health and wellbeing.
- Maintain information provided on FTSU intranet page on the Green Room and staff app, including details of the FTSU guardian, FTSU champions and how to raise concerns.
The FTSU guardians continue engaging with staff across the trust and working with champions to support the development of a culture where safety concerns are identified and addressed at an early stage. The FTSU guardians will continue working in 2022/23 to ensure more positive developments to FTSU, attitudes and behaviours across the trust, a healthy speaking up culture and role of the FTSU champions.
7.3. Learning from Deaths
Our Learning from Deaths processes have been firmly established since the inception of our policy on Learning from Deaths, and during 2021/22 we have delivered a robust process of reporting consistent with the requirements in the national guidance for ambulance trusts on learning from deaths published by the National Quality Board (NQB). This standardised and transparent approach to the reporting of learning compliments the quality improvement work within the trust and ensures we can protect future patients from avoidable harm, reduce unwarranted variation and provide truly patient-centred care.
NWAS has a dedicated cohort of senior clinicians within the trust who, following standardised training, undertake structured judgement reviews (SJR) monthly; these clinicians work alongside a multi-disciplinary team including representatives from the medical directorate, clinical quality, clinical safety, safeguarding and patient experience teams to enable robust reporting against the policy requirements. The structured judgement review methodology which is at the centre of our Learning from Deaths processes, allows us to identify strengths and weaknesses in the caring process and to provide information about what can be learnt about the systems and processes in use. It allows us to identify
where care goes well and to identify points where there may be gaps, problems or difficulty in the care process. To identify the strengths and weaknesses of individual patient contact episodes there is a need to look at the full range of care provided to an individual; this ‘end to end’ review of a care episode, from the point of call to the point of disposition, allows for the nuances of individual cases and the outcomes of interventions to be considered.
A key development in the Learning from Deaths processes during 2021/22 has been the engagement of our Patient Public Panel (PPP) in reviewing our processes and providing a patient and family centred critical review. This was the first of planned regular formal engagement with our PPP to ensure our Learning from Deaths processes are meeting the expectations of the patients, family, and carers we serve. A significant development will see PPP representation on the Learning from Deaths moderation panel meetings which will ensure we embed patient and family representation in the reviews we undertake.
Regular, formal quarterly reporting has been established and throughout 2021/22 we have met all reporting requirements with quarterly Learning from Deaths reports being received and reviewed through our corporate governance structure and ultimately by our Board for approval. Learning is also shared with the Regional Clinical Quality Assurance Committee.
The table below details the number of deaths reviewed and the number of deaths where problems in care have contributed:
| 2021/22Learning from deaths | Total Number of Deaths in scope | Total number of Deaths Reviewed | % Deaths Reviewed | Total number of deaths where problems in care havecontributed |
| Q1 | 68 | 46 | 67.6% | 18 |
| Q2 | 100 | 53 | 53.0% | 20 |
| Q3 | 163 | 71 | 43.6% | 29 |
| Q4 | Currently in progress | Currently in progress | Currently in progress | Currently in progress |
| Year-to-date | 331 | 170 | 51.4% | 67 |
Our approach to Learning from Deaths goes far beyond a process of simply counting, classifying, and reporting deaths; it is a commitment to supporting our journey towards providing an outstanding service to patients, their families, and carers.
The main contributory factors to patient deaths, where identified, were attributed to EOC procedures, specifically calls being incorrectly categorised and, operationally, a lack of available resources. The SJR process identified most patients received appropriate care, but where failings occurred these included the failure to record observations, details of clinical assessment and investigation findings together with the inappropriate application of clinical decision making and triage tools.
The SJR process has identified areas of good practice such as shared decision making and safety netting between clinicians the senior clinicians and where appropriate the patient’s general practitioner, whilst respecting the patient’s wishes to remain at home, crews showing care and compassion by allowing a natural death and supporting the family and caregivers in the process; and providing a detailed management plan to a patient within the community who is at risk of dying and refusing conveyance.
A commitment to disseminating and promoting good practice has been made by the consultant paramedic (medical) through the area learning forums and individual frontline staff.
7.4. Effectiveness
As set out in the Right Care strategy our goal is to provide clinically effective service using research evidence and agreed professional standards to improve clinical practice and service delivery through clinical audit, review, learning and improvement. In 2021/22 we set performance stretch targets relating to cardiac arrest and heart attack care which we are monitoring against national performance criteria, along with undertaking local workstreams such as understanding the impact of deprivation on cardiac arrest survival, the provision of social prescribing referral pathways and a detailed review of the triage decision support tools that are available for our clinical teams. This is to ensure that every clinical interaction receives the appropriate decision relating to care, and that we understand the impact of our interventions on a regional and local level.
7.4.1. The Ambulance Clinical Quality Indicators (ACQIs)
Our key measure of the effectiveness of our services is the National ACQI submission to NHS England. This is produced each month by the clinical quality team (quality management team) and used by clinical leadership to inform their local improvement and feedback to staff.
There are clinical leads for each of the indicators who lead working groups across the trust and work with system partners to learn and share outcomes. Local reporting on the National ACQIs is received quarterly at the trusts Quality and Performance committee and the Clinical Effectiveness sub-committee. Further localised reporting is provided to the clinical leads within the trust for cardiac arrest, STEMI, stroke and sepsis to contribute to learning and improvement in the quality of healthcare provided. The trust submits its ACQI outcomes and performance monthly as part of its National NHS England return.
Data collection for these indicators occurs three months in arrears, so the performance data displayed in the below tables are for April to November 2021. To note the cardiac arrest survival metric changed in January 2021 from cardiac arrest survival to discharge to cardiac arrest survival to 30 days, therefore there is no previous data for this data available.
| National AmbulanceClinical Quality Indicator | NovemberPerformance 2020/21 | NovemberPerformance 2021/22 | NovemberNational Average 2021/22 |
| Cardiac Arrest (All – ROSC at Hospital) | 27.6% (78/283) | 28.5% (92/323) | 24.3% (731/3004) |
| Cardiac Arrest (Utstein – ROSC at Hospital) | 45.2% (19/42) | 52.8% (28/53) | 45.6% (180/395) |
| Cardiac Arrest (All – Survival to 30 days) | Previously data submitted was Survival toDischarge | 8.0% (25/314) | 8.2% (242/2946) |
| Cardiac Arrest (Utstein – Survival to 30 days) | Previously data submitted was Survival to Discharge | 22.4% (11/49) | 26.0% (100/385) |
| STEMI PPCI Patients (Call to Angiography) | 02:21:00(141) | 03:00:00(109) | 02:40:00(897) |
| Confirmed Stroke Patients (Call to Door) | 01:24:00(616) | 01:51:00(522) | 01:52:00(4175) |
| Diagnostic Stroke Care Bundle | 98.5% (969/984) | 97.4% (856/879) | 96.9% (9040/9331) |
ACQI Outcomes (Q3 2020/21 – Q3 2021/22) Data Source: NHS England. 2021. Ambulance Quality Indicators 2021/22.
[ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-qualityindicators/ambulance-quality-indicators-data-2021-22/ [Accessed 14 April 2022]
Stroke Care Bundle
| Reporting Period: April 2021 – November 2021 | AQI Care Bundle Performance | NWAS: Outcomes from Stroke Care Bundle | National Average & Range |
| April 2021 | No National Data | Published | |
| May 2021 | 98.10% | 98.00% | |
| June 2021 | No National Data | Published | |
| July 2021 | No National Data | Published | |
| August 2021 | 97.80% | 97.80% | |
| September 2021 | No National Data | Published | |
| October 2021 | No National Data | Published | |
| November 2021 | 97.40% | 96.90% | |
| December 2021 | |||
| January 2022 | National data not | published at the time of | |
| February 2022 | writing | ||
| March 2022 |
ACQI Stroke Diagnostic Bundle data. Data Source: NHS England. 2021. Ambulance Quality Indicators 2021/22.
[ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-qualityindicators/ambulance-quality-indicators-data-2021-22/ [Accessed 14 April 2022].
Acute ST-elevation Myocardial Infarction Care Bundle
| Reporting Period: April 2021 – November 2021 | AQI Care Bundle Performance | NWAS: Outcomes from Acute ST- elevation Myocardial Infarction Care Bundle | National Average & Range |
| April 2021 | 77.70% | 77.40% | |
| May 2021 | No National Data Published | ||
| June 2021 | No National Data Published | ||
| July 2021 | 73.90% | 76.60% | |
| August 2021 | No National Data Published | ||
| September 2021 | No National Data Published | ||
| October 2021 | 60.10% | 74.20% | |
| November 2021 | No National Data Published | ||
| December 2021 | No National Data Published | ||
| January 2022 | National data not published at the time of writing | ||
| February 2022 | National data not published at the time of writing | ||
| March 2022 | National data not published at the time of writing |
ACQI STEMI Care Bundle data. Data Source: NHS England. 2021. Ambulance Quality Indicators 2021/22. [ONLINE]
Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulancequality-indicators-data-2021-22/ [Accessed 14 April 2022].
Post ROSC Care Bundle
| Reporting Period | AQI Care Bundle Performance | NWAS: Outcomes from Post POSC Care Bundle | National Average & Range |
|---|---|---|---|
| April 2021 | 61.3% | 77.0% | |
| May 2021 | No National Data Published | ||
| June 2021 | No National Data Published | ||
| July 2021 | 53.1% | 76.1% | |
| August 2021 | No National Data Published | ||
| September 2021 | No National Data Published | ||
| October 2021 | 65.0% | 77.5% | |
| November 2021 | No National Data Published | ||
| December 2021 | No National Data Published | ||
| January 2022 | National data not published at the time of writing | ||
| February 2022 | National data not published at the time of writing | ||
| March 2022 | National data not published at the time of writing |
ACQI Post ROSC Bundle data. Data Source: NHS England. 2021. Ambulance Quality Indicators 2021/22.
[ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-qualityindicators/ambulance-quality-indicators-data-2021-22/ [Accessed 14 April 2022].
| Reporting Period | AQI Care Bundle Performance | NWAS: Outcomes from Post POSC Care Bundle | NWAS: Outcomes from Sepsis Care Bundle | National Average & Range |
|---|---|---|---|---|
| April 2021 – November 2021 | ||||
| April 2021 | 61.3% | No National Data Published | 77.0% | |
| May 2021 | No National Data Published | No National Data Published | ||
| June 2021 | No National Data Published | 72.4% | 82.4% | |
| July 2021 | 53.1% | No National Data Published | 76.1% | |
| August 2021 | No National Data Published | No National Data Published | ||
| September 2021 | No National Data Published | 67.7% | 83.7% | |
| October 2021 | 65.0% | No National Data Published | 77.5% | |
| November 2021 | No National Data Published | No National Data Published | ||
| December 2021 | National data not published at the time of writing | |||
| January 2022 | National data not published at the time of writing | |||
| February 2022 | National data not published at the time of writing | |||
| March 2022 | National data not published at the time of writing |
ACQI Sepsis Care Bundle data. Data Source: NHS England. 2021. Ambulance Quality Indicators 2021/22. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulancequality-indicators-data-2021-22/ [Accessed 14 April 2022].
7.4.2. Reducing handover delays
In 2018, there were more than 700,000 attendances to hospitals across the North West by ambulance. In this period, it took on average 33 minutes from arrival at hospital to the point ambulance crews were ready for the next call. However, with wide variation in performance across the North West some average times were in excess of 40 minutes. In the same year 21,973 patients waited longer than 60 minutes for handover to hospital professionals. Hospital corridor queues were commonplace, resulting in poor patient experience, low staff morale, increased response times and serious incidents. 95,126 hours were lost from ambulances taking longer than the nationally prescribed maximum of 30 minutes for standard transfers. This equated to nearly 4,000 additional double-manned ambulances that would have been available in 2018. Therefore, a programme of improvement work to tackle delays called Every Minute Matters (EMM) was initiated and extended into a three-year programme of work with an aim of reducing average hospital turnaround time to the national standard of 30 minutes, with a stretch target of 26 minutes by 2021/22. At the end of phase two (year 2), 14 sites across the North West had participated, with 11 of the 14 sites showing a reduction in handover times, of three minutes per patient versus the baseline for the sites participating within the programme.
Phase three of this programme was due to start at the beginning of 2020/21, this was substantially redesigned and reduced in scope to support the pandemic response and this work has continued throughout 2021/22. This programme of work is aligned to and supports the ‘Six Point Plan’ for priorities ambulance, 111 and urgent and emergency care system winter improvement plan i.e. System and NWAS led initiatives of improvement in hospital handover times.
Key work that has been undertaken during 2021/22 includes:
- Continued involvement with the 3 acute sites who are part of the national NHSE/I hospital handover programme. These are Royal Oldham, Whiston and Morecambe Bay hospitals (Royal Lancaster and Furness General).
- Development of a training module which pulls together all the learning from the Every Minute Matters collaborative including videos, case studies and quality improvement models. The module is suitable for other acute and ambulance services to use. It has been tested by acute sites.
- Sharing hospital monthly data packs with hospital and commissioning leads to identify areas for handover improvement or to identify areas where improvements have occurred.
- On site quality improvement coaching at hospitals and with local NWAS teams to support the implementation of the ambulance handover safety checklist and escalation cards.
- Executive to executive conversations which focus on improving patient safety, addressing handover challenges, and sharing ideas for improvement.
- Joint work has been undertaken with Royal Preston emergency department to support the national NHSE/I pilot with 5 hospitals around the national rapid release policy which focuses on Category 2 patients waiting for an ambulance in Lancashire and South Cumbria. Multiple PDSA’s were tested, and learning shared with key stakeholders.
- Engagement at local, regional, and national forums sharing the work undertaken by NWAS to improve handover. This work was a HSJ 2021 finalist in the patient safety category.
Hospital handover delays have continued to be a challenge for Northwest Ambulance Services (NWAS) daily and have worsened during 2021/22. This picture has been reflected by other ambulance services across the UK. We have been working in partnership with emergency department teams, hospital senior management teams and with commissioners to address the handover challenges from a system perspective. Figure 6 below summaries our average turnaround time from April 2019 to March 2022.
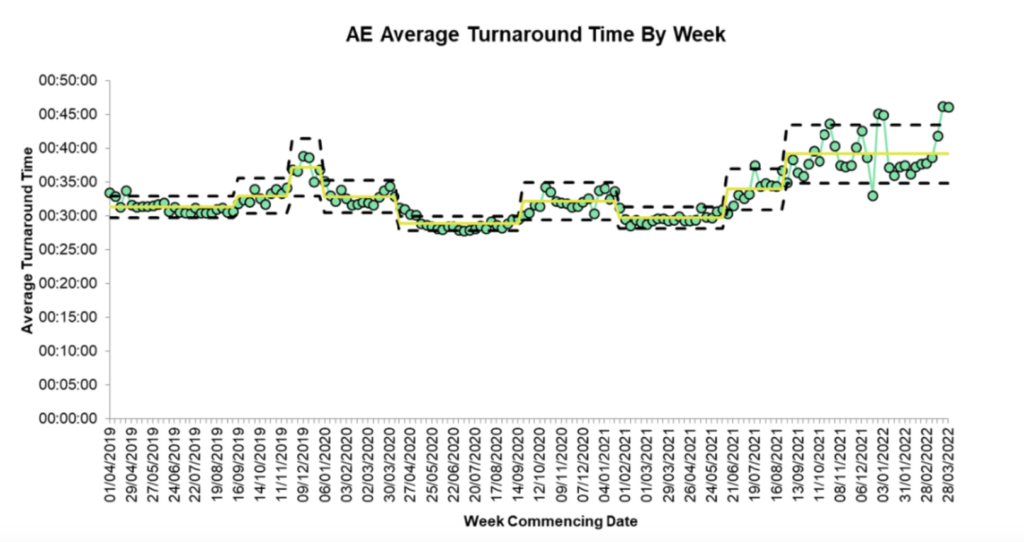
To support the challenges we face around handover NWAS has been developing an ‘Ambulance Handover Delays Managers Escalation action card’. The escalation action card was recently tested in collaboration with Bolton and Wigan emergency departments which proved successful during December 2021. Overall, the process was received well, crews were supportive of the approach and acute trusts found the process of collaborating to improve patient handover helpful.
The process has since been fully implemented in Greater Manchester acute sites during January 2022 and partially implemented across the remaining North West hospitals as part of a phased implementation process. Work is underway to complete implementation with the remaining emergency departments.
The purpose of the action card is to ensure:
- All hospital handover delays are managed in the same way and hospitals understand NWAS’s process for escalation.
- Any issues/risks are reported to the NWAS Regional Health Control Desk or senior executives where applicable.
- There is a clear process to de-escalate and return to normal state when issues have been resolved.
The implementation process has involved intensive engagement at both strategic and operational levels to roll out the escalation card to all North West emergency departments. It has required NWAS and hospital teams working through the action card in partnership.
7.4.3. Right Care at Home
The Right Care at Home work was aligned to the handover work where we have delayed admissions to maximise conveyance avoidance in those localities. During 2021/22 six NWAS sector teams were recruited to be part of this programme. This work was also aligned to NWAS’s Same Day Emergency Care (SDEC) and 2-hour urgent care response.
The collaborative aimed to reduce variation in practices by:
- Unlocking innovation: Sectors adopt an approach that empowers team members to suggest and test their own ideas for improvement and creates a climate where innovation blockers are challenged.
- Supporting confident decisions: Ensuring optimal application of triage tools to support safe and appropriate non-conveyance.
- Boosting clinical judgement: Extension of the clinical scope of practice in areas that are likely to support non-conveyance across many patients, e.g., wound care, dipstick urinalysis. This will be supported by learning what works for other ambulance trusts and the scope of practice of other NWAS clinicians.
- Developing smarter partnerships: Supporting clinicians to make full use of existing referral pathways by making sure they know what is available and can refer patients quickly and easily. This is intended to be focussed on building on existing relationships.
To support this work quality ambassadors were recruited from sector and to date there are 128 quality ambassadors. These roles are the project QI champions who lead quality conversations in sector around improvement opportunities. Before deciding what to focus QI interventions on audits were undertaken at emergency departments to identify opportunities. The audits identified the focus as:
- Service finder: To engage with NWAS staff through a quality conversation to increase the use of Service Finder for NWAS clinicians to improve See and Treat referral rates in sector.
- Action cards: To engage with NWAS staff through a quality conversation to discuss Hospital Handover Action Cards and obtain constructive feedback on the information provided.
- Alternative transport: To engage with NWAS staff through a quality conversation to increase the use of alternative transport for NWAS patients to hospital when appropriate and safe to do so.
NWAS sector teams then undertook PDSA cycles to test new ways of working. Learning has been shared across sectors.
7.4.4. Clinical Audit
The clinical audit team manages all aspects of the national mandatory clinical audits that related to patient outcomes as part of the ambulance quality indicator data sets. The data collected for this is detailed in section 7.4.1.
The introduction of an electronic report form, as part of the electronic patient record (EPR) has resulted in a mixed method of record keeping throughout the year. Gradually the paper record has been replaced with an electronic record which supports the clinician in offering pre-determined data entry (where appropriate) in addition to ‘free type space’ for more detailed data entry. The transition to electronic records has required iterative changes to the process for clinical data collection and audit. When paper records are completed, the audit is conducted using local databases. Where a record is electronic, the ambulance clinical quality indicator (AQI) identifier is located as a data field, and these can be retrieved from the electronic system as a list. The list captures all the appropriate AQIs, therefore the system is more reliable than using only the physical paper records as evidence to the number of AQIs undertaken by the trust. The audit interrogation of the list requires access to several systems and this in combination with the increased numbers has meant the trust has had to submit sample returns for certain ambulance clinical quality indicators (sepsis and stroke).
To improve the audit process and to access the benefits of the electronic report form process an in-house clinical audit tool is being developed. The development group is a multi- disciplinary team who include digital developers and specialists in the use of Power Business Intelligence (BI) systems working closely with the customer – the clinical audit team. The tool (Apex) is in phase 1 development – and the scope is to deliver an audit mechanism for each of the AQIs, with an output suitable for several audiences including the national submission requirements, and to frontline staff members as a personal clinical development indicator. At the time of writing phase 1 is mid-completion with Apex being in use for stroke and STEMI AQIs.
7.5. Digital
2021/22 saw our third year of delivery of the digital strategy focused on our goal to use digital solutions to radically improve how we meet the needs of patient and staff every time. Our work programme focussed on solving everyday problems using digital solutions, implementing new integrated critical systems, ensuring we have safe and resilient digital platforms, providing staff with the information they need to make the best decisions, testing new innovative ideas and developing progressive digital partnerships. We continued with the NWAS capital investment plan matched by significant external funding through the Unified Tech Fund to continue to upgrade our infrastructure and devices. Key achievements for 2021/22 included:
- Solving everyday problems: We have worked to ensure staff have the basics they need including upgraded Wi-Fi across all NWAS sites, new devices including personal issue ipads delivered to over 3,300 staff, a continued focus on supporting remote working and a programme of work to digitise key workforce and management processes starting with digital timesheets. We have received 49,548 service desk requests, successfully implemented 305 change requests for improvement across all services and significantly reduced the frequency of users having to re-open incidents.
- Our digital journey: We continued with our programme of work to replace our critical systems to enable our integrated urgent and emergency care strategy. This included completion of two major change programmes:
- 1. Unified Communications which saw the replacement of all telephony and communications platforms such as wallboards.
- 2. Completion of our EPR roll out including the ability to share EPR records with EDs before arrival. In addition, we made significant strides in enabling access to shared care records with the initiation of a project to enable a single access point to safely view and share patient information for the North West working with all ICSs and NHS E/I North. We also continued to build on our work to enable referrals to services through investment in the team that support that Directory of Services.
- Secure and joined up systems: We continued to improve email security with the implementation of Mimecast (an email security solution), ensured we are operating on supported platforms (8 remain unsupported) and increased our compliance with patching and carecert. We also continued our replacement programme for core infrastructure to make sure our systems are safe, reliable, and resilient. This was further supported by implementation of quarterly failover for critical systems.
- Smarter Decisions: We continued moving towards our goal to provide self-access data with the publication of 8 new Power BI outputs including real time performance dashboard, mental health, falls and maternity dashboards, a 111 report and IPC audit Dashboard. In addition, we developed a quality compliance scorecard which triangulates key quality and regulatory compliance measures and is reported monthly. Weekly reports were published from our SafeCheck system and we conducted an evaluation exploring how the system was adopted and used across the trust from which learning will feed in to phase 2 in 22/23. We responded to 365 requests for data and analysis between April 2021 and March 2022, whilst reducing average turnaround times from 21 days to less than 8 days in this period.
- Digital Pioneers: We continued to grow several partnerships to support our ambition to be digital pioneers including the University of Manchester, the Northern Ambulance Alliance, AACE digital transformation group and Alder Hey innovation centre. We also established and chaired the Ambulance Digital Innovation Forum. We continued to maximise the potential for our systems including being the first service to implement text messages with care advice from the 111 Cleric system. We tested and evaluated the SMART pilot which uses technology and process improvement to improve safety, efficiency and staff wellbeing. Our digital design forum which gives all staff access to the technical expertise and improvement support they need to test new digital ideas continued and we have done early work on a number of innovative areas including:
- Securing a partnership with NHS X to develop an algorithm to risk stratify the clinical queue.
- Delivering ‘mission interop’ using agile methodology to deliver the architecture to share information internally and across the Northwest – enabling safe access anytime, anywhere, any device.
- Developing a proof-of-concept proposal for the use of drone technology. Installing two new immersive reality training rooms to support enhanced training.
- Securing a partnership with NHS X to develop an algorithm to risk stratify the clinical queue.
7.6. Patient Engagement and Experience
Patient and Public Panel – Giving our patients ‘an increased voice’
Our Patient and Public Panel (PPP) was established in September 2019 to give patients, the public and communities a voice and the chance to have their views acted upon. The panel is made up of representatives from local communities, interest groups, the voluntary sector and partner organisations, and offers meaningful opportunities for members to influence decisions and improvements in our urgent and emergency care, patient transport and 111 services. The aim of the panel is to help support the delivery of safer services, improved patient and public experience and quality of care. Patients are experts in their experience and bring good knowledge of systems and how services work.
Despite the challenges from Covid-19, our PPP has continued to recruit new members and actively engage throughout the past 12 months via virtual platforms meaning we now have 213 Patient and Public Panel members fully inducted, with most already involved in the work of the trust. We hit our 2021/22 target of 190 for the PPP membership in the first half of the year, as well as doubling our aged 16-24 youth representation from the end of March 2021, which shows a great success for the trust.
The PPP has an infrastructure to enable patients/the public to become involved at a level that suits them, however at present, all levels are engaging virtually until further notice:
- Consult; is virtual, making the most of digital channels to interact with members who can get involved whenever or wherever they choose.
- Co-produce; panel members work together on short-term projects using co- production techniques.
- Influence; members take an ongoing, active role in high-level meetings to enhance decision making and discussions.
A breakdown of panel member’s involvement by level can be found at figure 7.
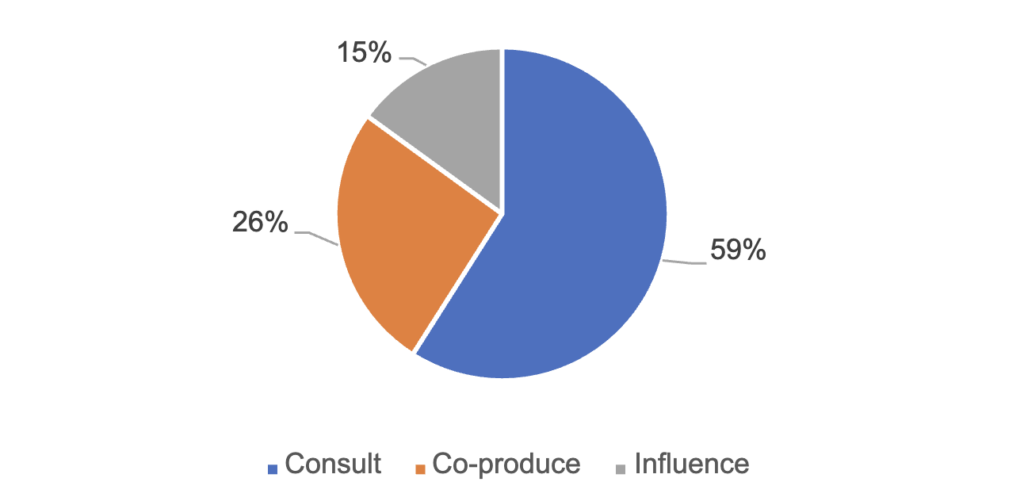
From April 2021 to March 2022, PPP members have been invited to get involved in 113 opportunities with 70 requests for panel involvement from staff across the trust.
The PPP have been able to get involved in regular meetings (area learning forums, Q&A sessions with the board, learning from deaths), development of the trust strategy as part of a reference group, medical markers review meetings, providing comments and feedback on the content. The membership receives regular information via a monthly newsletter, opportunities to engage with each other on a dedicated NWAS PPP members area and virtual development sessions (CPR, safeguarding). They have also had the opportunity to provide feedback on key documents and publications at the trust.
Panel members have been heavily involved in several quality improvement (QI) programmes at the trust, the development of the emerging new quality strategy to capture and ensure patient priorities were represented throughout. Members were invited to be involved in a Right Care at Home programme, working with NWAS staff to ensure patients who don’t need to go to hospital for emergency treatment receive the right care closer to home. First-hand patient experiences and written case studies from the PPP were included in a national NHS hospital handover training module about the difference care in the community had for them and their family. Inclusion of their experiences enhanced staff learning and empowered NWAS and other trusts to improve how they deliver effective QI programmes and improve ambulance care.
As already mentioned, we have successfully reached our 20% target which is currently 22% for members in the younger age bracket (16-24) as shown at figure 8. However, we recognise more work needs to be done to engage with young people across the North West. The trust has secured funding to further progress recruitment of young people to become NWAS PPP panel members and the ongoing development of a youth zone on the trust’s website during 2022/23.
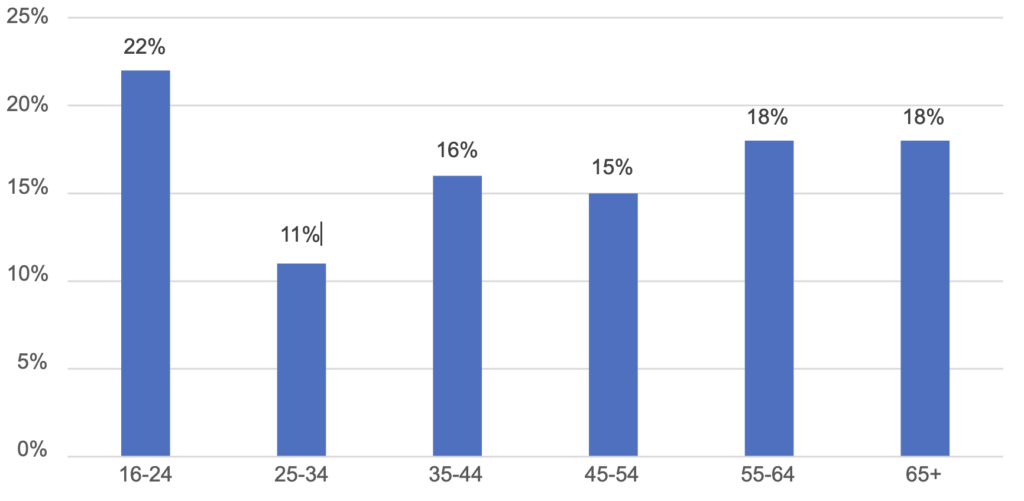
Patient feedback including Friends and Family Test 2021/22
An extensive patient engagement programme was successfully completed during 2021/22. In addition, to our NHS 111 postal survey offer and FFT comment/postcards on vehicles, we continue to develop our digital offer by offering the opportunity to complete our patient surveys via a SMS text weblink and online https://www.nwas.nhs.uk/get-involved/share- your-experience/tell-us-how-we-did/ Also, instead of the traditional face to face engagement that would normally take place with patient, health practitioner networks, forums and community groups, we now attend these across virtual engagement sessions via MS Teams and Zoom.
New guidance for the FFT came into force from 1 April 2020 and although reporting had been delayed by NHS England due to the impact of Covid-19, national reporting recommenced during 2021/22 with a continued focus on digital channels via SMS text. Figure 9 and 10 below respectively provide a summary of survey response feedback data including FFT by quarter.
Patient Engagement Surveys(01 April 2021 – 31 Mar 2022) | Patient Transport Service | Paramedic Emergency Service | Urgent Care Service | NHS 111Service | NHS 111First Service | |
| Q1 | 1 | 2 | 1 | 620 | 423 | |
| Q2 | 13 | 10 | 0 | 454 | 534 | |
| Completed PE Surveys | Q3 Q4 | |||||
| 248 | 248 | 36 | 333 | 406 | ||
| 439 | 349 | 120 | 589 | 509 | ||
| YTD | 701 | 609 | 157 | 1,996 | 1,872 | |
| Cared for appropriately with | Q1Q2 | 100% | 100% | 0.0% | n/a | n/a |
| 76.9% | 90.0% | No Data | n/a | n/a | ||
| 94.4% | 90.7% | 77.8% | n/a | n/a | ||
| Dignity, Compassion | Q3 | |||||
| and Respect | Q4 | 94.6% | 94.6% | 84.2% | n/a | n/a |
| (Strongly Agree/Agree) | ||||||
| YTD | 94.2% | 92.9% | 82.2% | n/a | n/a | |
| Q1 | n/a | n/a | n/a | 91.6% | 95.0% | |
| Overall Satisfaction | Q2 | n/a | n/a | n/a | 89.6% | 92.8% |
| Received(Very Satisfied/Fairly Satisfied – Yes) | Q3 Q4 | |||||
| n/a | n/a | n/a | 84.4% | 92.1% | ||
| n/a | n/a | n/a | 88.3% | 91.2% | ||
| YTD | n/a | n/a | n/a | 89.0% | 92.7% | |
| Overall Experience of | Q1 | 100% | 50.0% | 0.0% | 91.8% | 93.3% |
| 61.5% | 80.0% | No Data | 91.4% | 87.4% | ||
| Service / Recommend | Q2 | |||||
| Ambulance Service to Friends andFamily(Very Good/Good – Extremely | Q3 Q4 | |||||
| 87.1% | 87.1% | 47.2% | 88.0% | 85.7% | ||
| 90.0% | 87.1% | 62.5% | 90.0% | 85.4% | ||
| YTD | 88.5% | 86.9% | 58.6% | 90.5% | 87.9% | |
| likely/Likely) | ||||||
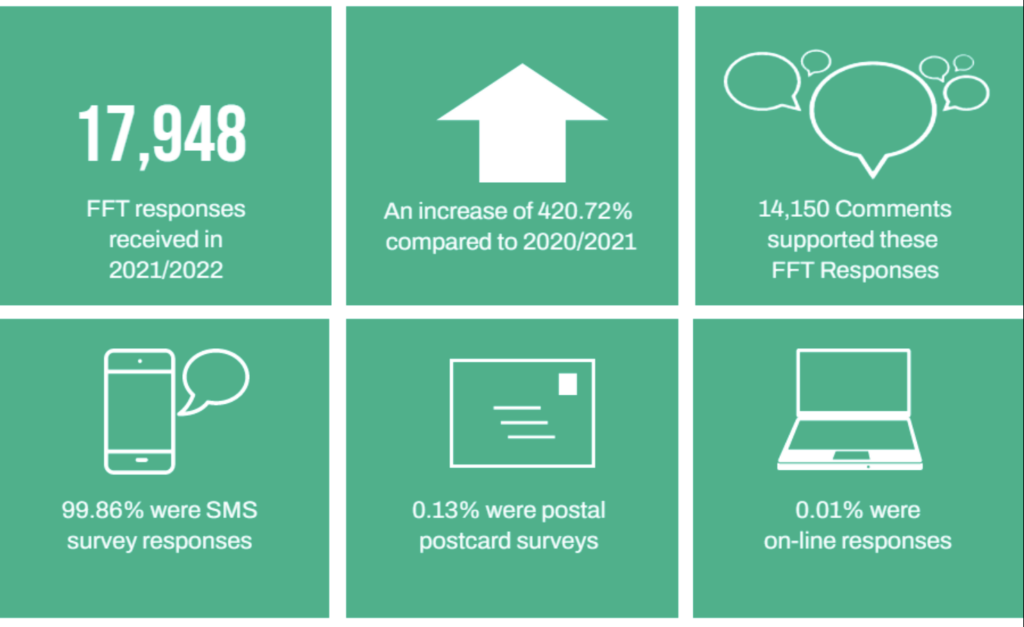
Community Engagement Guidance Framework 20/25
Overarched by our trust Community Engagement Guidance Framework 20/25 the trust
adopted a patient, public and community engagement implementation plan for 2021/22. The
plan highlighted the need for flexibility and creativity of approach to community engagement
presented by the Covid-19 pandemic to continue to gather real insights into the care and
treatment that patients have received.
During 2021/22, we engaged virtually with several patient and community groups on a range
of topics, one was to talk about our response during the Covid-19 pandemic, trust plans for
moving out of lockdown with PTS services and use of escorts and to reassure communities
that they were safe when using Ambulance services. Another focus for engagement was
the importance of using NHS111 first and talking to groups about the range of options to
access that service and the other services that NWAS provides.
More than 84 virtual engagement events were attended by the trust as either principal
speakers, advisory or facilitators. Virtual patient and public community engagement events
included: Salford Mental Health Forum, Healthwatch, Blackpool Learning Disability Group,
Black History Month activities, Caribbean and African Health Network, Dementia Café and
CCG conferences. Our engagement has looked slightly different to previous years as many
of the ‘face to face’ high footfall events that we would usually attend such as Freshers Fairs,
Disability Awareness Days and PRIDE were cancelled due to the pandemic. During 2022/23
we will continue our cautious approach to resuming face to face engagement where an
appropriate risk assessment allows and where restrictions are lifting.
Themes
Feedback has demonstrated a general high regard for the ambulance service and in
particular the high percentages of patients feeling they were treated with dignity compassion
and respect whilst identifying specific themes, which will be further analysed and articulated
as recommendations for improvements during 2022/23. Some of these themes include:
â– Communication: Feedback from our deaf community has highlighted the increased
barriers to lip reading communication due to our staff wearing personal protective
equipment (PPE) during the pandemic. Ways in which we have looked at breaking
down those barriers have already included the procurement of deaf awareness
training for 50 staff members. During 2022/23, staff will be provided an opportunity
to download an ‘Insight’ language communication App on their ipads. This will
ensure provision of language translation as well as BSL translation support at patient
side. We will continue to ensure that any videos that are shown on social media are
subtitled, and our Virtual AGM was signed by a BSL interpreter.
â– Reassurance: We provided reassurance to our patient, public and community
groups throughout and during lifting of the pandemic restrictions, regarding
resources, safety of our services, availability, and our overall response to the
pandemic via regular stakeholder updates, patient engagement events and
information bursts. We also kept them informed on an area-based perspective of
the availability of local services to support their self-care, with mental health as well
as physical health and well-being respectively. We sent 11 sets of info-bursts
including: How to protect yourself in the hot weather, Winter watch, Covid-19
restrictions information and mental health resources by county area. This is a key
area of trust activity that will be maintained throughout 2022/23.
â– Accessibility: Following feedback that despite using Microsoft Teams for most of
our engagement, Zoom is much more accessible for those with additional
accessibility needs, we purchased a Zoom licence to undertake engagement and
meet the needs of this group of patients. We will continue to share co-produced
information on how our emergency services are accessed using emergency SMS 999 British Sign Language (BSL) to be introduced summer 2022 and how NHS111 can be accessed using the services of Co- Sign (Interpreter Now).
â– Co–Production: Further to co-production work with the PPP already undertaken on
a new pictorial communication handbook, this will now be progressed to a digital
version for staff to upload on to new ipads. Consideration will be provided to similar
with a digital version of the Multilingual Phrasebook to further enhance
communication with ethnic minority ‘new’ communities in the region. Patient
Engagement FFT feedback, learning and related themes will be co-designed for
improvements with trust service line ambassadors for PTS, PES and NHS 111
services.
â– Information: Following feedback that we need to make our publications more
accessible; PPP information is now always provided in an accessible format for our
visually impaired members and those who require their information in high contrast.
We also have also invested in a photo symbols subscription so we will be able to
produce more easy read information in the future. Monthly newsletter support will be
continued throughout 2022/23 for our PPP membership.
â– Engagement: Overarched by the trust patient, public and community engagement
guidance framework for 2020/25, we will ensure a minimum 1% of PTS, PES See
and Treat, and 1,200 NHS 111 patients receive the opportunity to provide FFT
feedback monthly. Our recent review of the patient engagement reporting platform
IQVIA will support Northwest areas, towns and cities-based understanding with
patients survey feedback and well as by demographics.
We will take into account the learning from Covid-19 safe patient engagement during
2021/22 as well as central and local guidance in particular on continued virtual engagement
e.g. accessibility, ease of travel, time etc to inform our annual Patient Engagement
Implementation Plan for 2022/23. Further to recent Government advice for attending large
scale events. We are starting to receive large scale events invitations for some events
already for summer 2022 We will undertake appropriate risk assessments and proactively
scope NWAS attendance at e.g., Disability Awareness Day, Manchester Pride and Health
Mela invites
7.7. Pillars of quality
We improve quality continuously using our ‘pillars of quality’ listed below:
â– Complaints and Compliments
â– Incident reporting (including serious incidents)
â– Health, safety and security
â– Infection prevention and control
â– Medicines management
â– Safeguarding
7.7.1. Complaints and Compliments
Complaints 2021/22
The trust embraces all feedback from patients, including those whose experience has not
met their expectation and so has been raised through the complaints process. Complaints
provide us with opportunities to investigate what has happened and identify and implement
lessons learnt. Learning can be at an individual and/or a system wide level.
In the NHS complaints are categorised into complaints which are those received directly
from a patient, or their relatives and a category termed externals which are complaints
received from a third party such as other health care professionals, nursing homes and other
emergency services.
Number of Complaints
From 1 April 2021 until 31 March 2022, the trust received 2,180 complaints (an average of
182 complaints per month). Comparison data for complaints is included from the previous
two financial years:
| Year | Complaints | Externals |
| 2019/2020 | 2023 | 1435 |
| 2020/2021 | 1346 | 993 |
| 2021/2022 | 2180 | 1726 |
We are not able to draw direct comparisons with 2020/21 as it was the first year of the Covid-19 pandemic including national lockdowns. A more helpful comparison is with complaint data from 2019/20 which indicates that there has been an increase of 20%.
We are not able to draw direct comparisons with 2020/21 as it was the first year of the Covid-19 pandemic including national lockdowns. A more helpful comparison is with complaint data from 2019/20 which indicates that there has been an increase of 20%.
Complaints Process and Risk Categorisation
The increase in complaints created an associated impact on the ability of the Patient Safety team to manage the complaints within agreed timescales. Additional support and focus were given to that team to mitigate the increased case load. The status of complaints that were received for the referenced period is:
| Complaints received for the period 1 April 2021 until 31 March 2022 | |||
| Ongoing: | Upheld: | Partly Upheld: | Not Upheld: |
| 261 | 333 | 376 | 1210 |
All complaints are risk scored using the trust risk matrix. High risk scores (level 4-5) are presented to the Review of Serious Events (ROSE) group. They are the decision-making panel for reporting of serious incidents on the national Strategic Executive Information System (StEIS). Complaints recorded as a StEIS are thoroughly investigated in line with the investigation teams terms of reference.
When moderate or severe patient harm has occurred, the trust are committed to enacting Duty of Candour. This includes sharing investigation findings with patients, their families and / or representatives. The table below shows the breakdown of complaints into their risk categories.
| Level | Q1 | Q2 | Q3 | Q4 | TOTAL |
| Level 1-2 | 421 | 469 | 399 | 346 | 1,635 |
| Level 3 | 88 | 156 | 107 | 76 | 427 |
| Level 4-5 | 26 | 26 | 33 | 33 | 118 |
| Total | 535 | 651 | 539 | 455 | 2,180 |
Assurance
Governance structures ensure data are scrutinised and assurance is given on delivery of
the service and incorporation of learning in service improvement plans. The Quality and
Performance committee and the Board of Director receive information on complaints
through a bi-monthly integrated performance report.
A new Patient Safety sub-committee was established in May 2021, reporting to the Quality
and Performance Committee. The Patient Safety sub-committee seeks assurance relating
to patient safety activities within the trust, especially those referenced within the National
Patient Safety strategy and the NWAS Right Care (Quality) strategy. A key element of this
committee is that of the Patient Story in which a patient complaint is presented on their
behalf or indeed by the patient or relative themselves. These stories serve as a powerful
reminder that the patient must be at the centre of everything we do.
On a monthly basis NWAS meet with commissioners, patient representatives, external
clinical and quality leads to discuss quality and safety agendas via the Quality and Safety
group and Regional Quality Assurance meeting.
Parliamentary and Health Service Ombudsman
The trust has an agreed Redress Procedure to provide guidance on questions of remedy in
line with the guidance provided by the Parliamentary and Health Service Ombudsman
(PHSO) for reasonable, fair, and proportionate remedies during its complaints handling
processes. All complaints are advised of their right to appeal if they are unhappy with a
complaint response and details of the PHSO are included in our written responses. This
year 2 cases were brought before PHSO and neither were upheld. Low levels of concerns
raised to PHSO and upheld signals robust systems to complaints management.
Learning
Learning Forums receive, review, synthesise and share the learning identified from
complaints investigations. A review of those complaints established that the six most
common reasons for complaints throughout 2021/22 has been:
â– Emergency response (29%)
â– Staff conduct (18%)
â– Care and treatment (17%)
â– PTS journey times (17%)
â– Communication and information (10%)
â– Driving standards (3%)
These common reasons are broken down into their assigned risk categories:
| Theme / Level | 1Minimum | 2Minor | 3Moderate | 4Major | 5Serious | TOTAL |
| Emergency Response | 22 | 274 | 263 | 63 | 19 | 641 |
| Staff conduct | 166 | 211 | 20 | 0 | 0 | 397 |
| Care & Treatment | 31 | 215 | 109 | 28 | 5 | 388 |
| PTS journey times | 73 | 300 | 9 | 0 | 0 | 382 |
| Communications & information | 95 | 114 | 26 | 2 | 1 | 238 |
| Driving standards | 49 | 32 | 0 | 0 | 0 | 81 |
We triangulate information from complaints with incidents, performance data, claims and legal data to gain further insight and opportunities for learning. This year we have presented a deep dive paper to our executive leadership team outlining learning and plans to strengthen the team in 2022/23 with the integration of the complaints team into the corporate governance team.
Compliments
1410 compliments were received during 2021/22 from across all areas of the geographical footprint. This was an increase of 65 compliments since 2020/21. During June 2021 a new system for recording compliments was introduced called Datix Cloud IQ. This system has lots more functionality to collect more detailed information about compliments.
7.7.2. Incident Reporting (including all serious incidents)
Serious Incidents 2021/22
In 2021/22 we have continued to manage Serious Incidents via robust arrangements. On the identification of a risk score 4 or 5 incident, this is presented for consideration at the trust’s Review of Serious Events (ROSE) Group, which meets weekly and is chaired by the Medical Director or nominated deputy. The membership is comprised of senior clinicians, and subject matter experts. The lead Commissioner’s patient representative has also continued to attend to provide a valued patient perspective as part of the process.
On declaration of a Serious Incident, a Duty of Candour Lead and appropriately trained Investigating Officer is allocated. The investigation is conducted with input from our healthcare partners as part of the investigation as required, subject matter experts and engagement with the individual affected or significant others. In 2021/22, members of the Patient Safety Team have completed the Healthcare Safety Investigations Branch (HSIB) level 3 training to ensure that our investigations focus on not only organisational learning, but wider systems learning. Throughout the process, there are a number of assurance processes to ensure we have fully met the terms of reference and maximised the opportunity for learning & transparency.
The Quality and Safety Group and Regional Clinical Quality Assurance Committee (RCQAC) review each individual serious incident and ensure that learning from incidents is embedded within the trust before the incident is formally closed.
Within 2021/22, 514 level 4 and 5 cases have been considered at ROSE. Of these, 86 cases (17%) were deemed to reach the threshold for reporting as a serious incident and were reported by NWAS to the commissioners via the Strategic Executive Information System (StEIS). A small number of these 514 cases will have been presented to ROSE on more than one occasion when further information has been confirmed.
Analysis of the data has shown a 72% increase in comparison to the previous year (50 declared in 2020/21) in the number of cases being identified as reaching the threshold for reporting as a serious incident (SI). This is largely attributed to a rise in demand for higher acuity calls, and a continuous improvement in our reporting and safety systems (many of our incidents are internally / self-reported).
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 2019/2020 | 7 | 14 | 12 | 14 | 47 |
| 2020/2021 | 13 | 12 | 15 | 10 | 50 |
| 2021/2022 | 10 | 18 | 23 | 35 | 86 |
The breakdown of origin or location of the cases are as follows:
| Area | Number |
| EOC Cumbria and Lancashire | 20 |
| EOC Greater Manchester | 18 |
| EOC Cheshire and Mersey | 18 |
| PES Cumbria and Lancashire | 6 |
| PES Greater Manchester | 12 |
| PES Cheshire and Mersey | 3 |
| PTS | 2 |
| 111 | 6 |
| Trust wide | 1 |
The reason for reporting harm were due to the following broad categories:
- Delayed response
- Care and treatment provided
- Information and communication issues
- Equipment issues
All serious incidents are subjected to investigation under the NHS Serious Incident Framework and as required, are reported in full to commissioners. Through established working arrangements, the trust and its commissioners worked closely together throughout the year to ensure that action plans to learn appropriate lessons and to prevent the recurrence of serious incidents are in place and accomplished.
In 2021/22 we have identified and begun to implement both organisation and system learning from Serious Incidents:
- Review of service model to maximise resources available to incidents.
- Working closely with our acute partners to reduce handover delays maximising resource in community.
- Continued training for staff in our Emergency Operations Centre to recognise priority symptoms.
- Introduction of NHS Pathways across the NWAS Emergency Operation Centres (a new call triage system).
- A requirement to strengthen processes and procedures relating to non-conveyance of patients, with education and training to support.
- Education and communication around specific clinical subjects for example, interpretation of electrocardiograms.
- Strengthening processes around end-of-life care, for example, administration of medication.
- Working with system partners to improve pathways and support for patients presenting with mental health conditions.
The learning identified through serious incident investigations is embedded in several ways:
- Via area learning forums
- Clinical contact shifts
- Education and training (mandatory and essential)
- Communications and bulletins
- Planned exercise (e.g., major incident exercise)
- Changes to written policy and procedure
We have also strengthened our governance arrangements via our sub-committees to triangulate intelligence from incidents, complaints, compliments, and coroners’ inquests, in addition to proactively seeking to learn from intelligence in organisations to prevent occurrence in our trust.
Regulation 28
NWAS received one Regulation 28 report from HM Coroner in 2021/22. NWAS expects to receive a very low number of Regulation 28 reports as it proactively and continuously seeks opportunities for improvement and to ensure that any/all learning actions which may arise from a coroner’s investigation are completed in a timely manner.
Incidents 2021/22
In 2021/22 NWAS have reported 16,471 incidents in total. This is broken down by risk score:
- Risk 1 (low) – 1,809
- Risk 2 – 8,881
- Risk 3 – 5,247
- Risk 4 – 206
- Risk 5 (high) – 103
- Not risk scored – 225
In terms of our activity over the year, with 1,799,668 contacts incidents occurred in 0.9% of these. We actively encourage a culture of reporting so that we can learn from incidents.
| Incidents by Type | Number of Incidents |
| Clinical Incident | 1910 |
| Clinical Near Miss | 507 |
| IM&T / IG Security | 132 |
| Non Clinical Incident | 629 |
| Non Clinical Near Miss | 481 |
| Patient Injury | 317 |
| Public Injury | 36 |
| Staff Injury | 2582 |
| Raise an Issue / Concern | 4375 |
| Raise a notification | 720 |
| 111 | 3634 |
| Not Categorised | 1148 |
Learning
Learning is identified and disseminated in the following ways:
- Patient Stories
- Area Learning Forums
- Changes to policy & Procedure
- Staff education
- Communications e.g., bulletins
- In 2021/22 there has been significant work done around violence and aggression, medicines management, moving and handling and IPC because of incident learning.
- It is hoped that with the implementation of the Datix Cloud IQ reporting system, we will be able to identify themes and learning much easier as these will be more meaningful data
- fields rather than free text. Incidents have now moved into the risk portfolio which enables us to triangulate information more efficiently.
7.7.3. Safeguarding
The trust has a statutory responsibility to safeguard children and adults who are at risk of harm from abuse or those who are vulnerable, this commitment is underpinned by specific legislation, namely Children’s Act (1989 & 2004) and the Care Act (2014). The trust works in partnership with other organisations to ensure that the response to individuals who are at risk of harm from abuse or neglect or who are vulnerable, is communicated in an effective manner which results in an appropriate response.
Safeguarding activity
2021/22 has seen safeguarding figures fluctuate during the early part of the year, this has been attributed to the Covid-19 pandemic. The table below details the activity:
| Concern raised | Apr – 21 | May – 21 | Jun – 21 | Jul – 21 | Aug – 21 | Sep – 21 | Oct – 21 | Nov – 21 | Dec – 21 | Jan – 22 | Feb – 22 | Mar – 22 |
| Adult | 5978 | 6061 | 5308 | 5037 | 4880 | 4503 | 4267 | 4223 | 4254 | 4547 | 4228 | 4375 |
| Child | 1217 | 1372 | 1119 | 939 | 762 | 856 | 768 | 820 | 717 | 814 | 852 | 832 |
| Total | 7195 | 7433 | 6427 | 5976 | 5642 | 5359 | 5035 | 5043 | 4971 | 5361 | 5080 | 5207 |
Work undertaken in 2021/22
- Private providers assurance reports gained from all 19 private providers in relation to safeguarding, reflecting training, DBS compliance, policies and procedures and governance.
- The NWAS support centre were all trained on use of the Cleric system during 2 days of intensive training.
- All safeguarding and maternity alerts are now placed onto the Cleric system.
- 4 bespoke safeguarding/early help forms have been designed in collaboration with social care partners and will be used on the Cleric system when it goes live.
- Two bespoke safeguarding e-learning packages have been written and developed and are now live.
- Carers pathway was designed and launched across the trust, providing guidance to all staff to ensure some of the most vulnerable members of our communities are protected.
- Delivered training to support level 3 learning outcomes to paramedic workforce to support transition to new requirements under the intercollegiate documents.
Safeguarding Systems Review
With the continually increasing safeguarding numbers a review of the current systems used was necessary. ERISS is the system, which is currently used, it was identified that the system is expensive to maintain and develop further, a working group was setup to review this and operated under the title of Project Emerald.
Project Emerald will see a whole system change from the current electronic referral information sharing system (ERISS) system to the Cleric system. The Cleric system will allow for more accurate data collection and reporting and will allow the Safeguarding team to monitor rejections and feedback in a more accurate manner. The testing phase of this project is expected to start in the early summer of 2022 and over 1 million postcodes have already been put into new system in preparation of the testing.
Safeguarding Board Engagement
Increased notifications, improved visibility and Board engagement has resulted in increased numbers of requests to be involved in Safeguarding Adult Reviews, Domestic Homicide Reviews, Serious Case Reviews, Learning Disability Reviews and Strategy Meetings.
The Safeguarding team work alongside senior managers and clinicians to ensure engagement with the Boards is visible and specific to local needs. There are currently 46 safeguarding boards across the geographical footprint of North West Ambulance Service and the team have committed to attend each board a minimum of once per year, or, as per local board request. Board engagement is monitored by the Safeguarding team. In addition, practitioners and managers are involved in local safeguarding board sub-groups. Engagement includes:
- Child Death Overview Panel
- Rapid Response meetings
- Alternative Life Threatening Event meetings
- Basic Learning Reviews
- Serious Case Review groups
- Safeguarding Adults Review groups
- Domestic Homicide Reviews
- Front line visits with local board members
- Wider stakeholder meetings
- Integrated Care System meetings
- Multi-agency review meetings following the Sudden Unexplained Death of a Child (SUDC)
Serious Case Reviews, Safeguarding Adult Reviews and Domestic Homicide Reviews (DHR)
During the 2021/2022 year the safeguarding team were involved in 229 safeguarding reviews, these are broken down into 112 adult reviews, 71 child reviews and 46 domestic homicide reviews. In direct comparison 2020/21 saw the team engaged in 256 safeguarding reviews. Although there has been a reduction in adult and child reviews the number of domestic homicides during the past year has almost doubled in number. The safeguarding team will continue to analyse cases and data to identify any themes or learning.
Learning is captured for each organisation involved within the individual reports where applicable. Any learning specifically for NWAS or that can be applied to the trust is recorded on the safeguarding learning tracker. Learning for these cases is then disseminated through the corporate learning forum, the regional learning forums, directly with the staff involved and trust wide via the weekly regional bulletins and built into the mandatory training scenarios.
7.7.4. Health, Safety and Security
NWAS is committed to ensuring a safe system of work approach to health, safety, and security (HSS) and has put in place the organisational arrangements necessary to fulfil its statutory and mandatory obligations. We look to prevent workplace/related injuries, ill health and protection of staff, property, and assets by promoting good working practices. All staff are responsible for ensuring that they follow policies and procedures to keep themselves and their colleagues and patients safe at work. Our HSS work is done in partnership with trade unions who are full members of the sub-committee and work with service lines on local health and safety management.
The Health, Safety and Security A-Z Toolkit supplies guidance on how relevant legislation should be interpreted and used in NWAS. It is a ‘live’ toolkit and subject to regular review. Each document is subject to review and consultation before approval. In 2021/22 the following policies, procedures and guidance have been reviewed:
- Health and Safety policy
- Reduction of Violence and Aggression policy
- Manual handling procedure
- Complex needs pro-forma
- Risk assessment for patients own wheelchair electric/manual
- Manual handling risk assessment: additional information
- Slips, trips and falls
- Generic risk assessment: GRA 014 Community Paramedic
- Generic risk assessment: GRA005 Observer
Regulatory Activity
NHS (National Health Service) Trusts HSS systems are regulated by at least three regulatory bodies:
- Care Quality Commission (CQC)
- Health and Safety Executive (HSE)
- Medicines and Healthcare products Regulatory Agency (MHRA)
Reporting of Injuries, Diseases and Dangerous Occurrences Regulations (RIDDOR) National RIDDOR reporting requires the activity to be reported using the methodology of number of incidents per 1,000 staff. The number of staff employed as at 31/03/2022 is 7358 (includes bank staff); and the number of staff injury RIDDORs reported in the 12 months to 31 March 2022 is 130. The total number of journeys (PTS and PES) combined is 1, 021,462 (PES) for the same period.
The incident rate of RIDDOR reporting is calculated as 17.5 per 1,000 staff members, which when compared against the incident rate per 1000 staff for the previous year has increased slightly by a factor of 0.09.
The incident rate is calculated as less than 0.1 staff injuries per 1,000 staff journeys.
The national RIDDOR comparison rate for 2021/22 is not available at the time of writing this report, and in its absence for the purposes for this report the 2020/21 ambulance sector averages are as follows for comparison.
| AmbulanceSector Average 2020/21 | NWAS RIDDORrate 2021/22 | |
| Incident Rate (Injuries x 1000 ÷ No of Journeys) Staff injuries only | 0.11 | 0.1 |
| Incident Rate (Injuries x 1000 ÷ No of Employee) Staff injuries only | 19.38 | 17.5 |
RIDDOR rate 2021/22
Non-clinical incident activity
A non-clinical incident is identified as any incident recorded in the incident reporting system categorised in any of the following categories:
- Raise a concern
- Raise a notification
- Staff injury
- Patient injury
- Public injury
- Non- clinical incident
- Non-clinical near miss
The table below summarises the non-clinical incidents reported for the 12 months to 31 March 2022, and it describes that across each directorate there is active non-clinical incident identification and recording.
| Non-clinical incidents by Directorate | Q1 21/22 | Q2 21/22 | Q3 21/22 | Q4 21/22 | Total |
| Service Delivery Directorate (PES, EOC, UCS, PTS etc.) | 2906 | 2477 | 3017 | 2717 | 11117 |
| Medical Directorate | 44 | 47 | 46 | 44 | 181 |
| Finance Directorate (Finance/Fleet/Estates etc.) | 16 | 13 | 10 | 18 | 57 |
| Quality Directorate | 7 | 10 | 9 | 10 | 36 |
| People Directorate | 8 | 5 | 9 | 19 | 41 |
| Corporate Affairs Directorate | 1 | 3 | 2 | 4 | 10 |
| Strategy, Partnership and Transformation Directorate | 4 | 4 | 3 | 6 | 17 |
| Board of Directors | 0 | 0 | 0 | 1 | 1 |
| Total | 2986 | 2559 | 3096 | 2819 | 11460 |
The number of non-clinical incidents reported has increased by 65% since 2019/20. The increase in reporting represents positively the identification of incidents and this; on its own; does not constitute a risk or issue as staff are encouraged to record concern and near miss incidents.
Non-clinical incident themes
Analysis of the themes from non-clinical incidents arising in the year to 31 March 2022 have identified the following ‘top 3’ most reported.
- Equipment missing, damaged, lost, stolen or fault: 897
Staff have reported increasing amounts of equipment missing, et al. A review of this data has identified there are three subcategories: equipment identified as missing or lost (312), equipment failure – including at test and at scene (291) and equipment damaged – including accidental and third party (254). - Access, admission, transfer: 1,031
The access, admission and transfer theme can be largely attributed to the delay in gaining access to hospital, where an ambulance crew is delayed with the patient in the vehicle; of the reported non-clinical incidents 792 were categorised in this way. - Violence and aggression incidents: 1,567.
The worrying number of violence and aggression incidents across the NHS has prompted supportive activities in the ambulance sector for staff who have or may be risk of such incidents. One such is the national #WorkWithoutFear campaign – led by the Association of Ambulance Chief Executives with support from NHS England and NHS improvement (www.aace.org.uk/vaa). The campaign highlights the impact of abuse on ambulance staff whilst encouraging the perpetrators of the abuse to have respect for those who are trying to help them. Further details of the improvement work to reduce violence and aggression is detailed below.
Reducing Violence and Aggression
The World Health organisation defines violence as ‘the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or a community that either result in or has a high likelihood of resulting in injury, death, psychological harm, mal-development or deprivation.’ (Global status report on violence prevention, 2014).
NWAS finds deliberate violence and aggression towards our staff or people who use our services unacceptable. Where violent or aggressive behaviour may occur due to clinical and or medical factors, all possible primary and preventative measures should be used to reduce the prevalence and risk of harm. Patient facing staff (including 111) have reported 1,567 incidents of violence and aggression in 2021/22. Split into three main categories the incidents occurred as follows:
- Physical assault: 401 incidents
- Threatening Behaviour: 506 incidents
- Verbal Abuse: 660 incidents
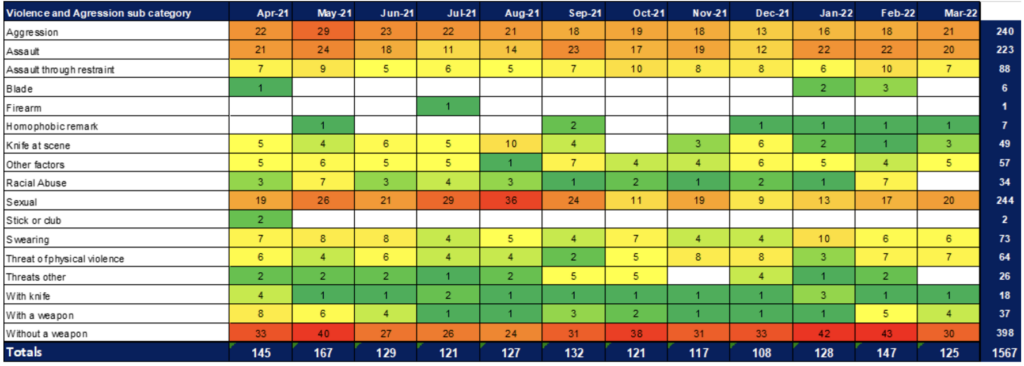
In response to the national security standards released in December 2021, NWAS has developed a Violence Prevention and Reduction policy whose purpose is to create a culture ensuring NWAS is and still is engaged in and driven to provide:
- Positive and proactive care to the people who use our services, and
- Create a supportive and safe environment for staff to work in
A key element to support the prevention and reduction of violence and aggression activity is the self-assessment document associated with the national standards. The standards describe the activities that will support the reduction of violence and commits to keep staff safe in the workplace. The NWAS violence prevention and reduction group takes part in the self-assessment and is the vehicle to support activity needed in closing the gaps to meet the standards set.
Body worn cameras
There are national commitments from NHS England to reduce violence and aggression towards NHS staff as outlined in the NHS Long Term Plan. NWAS are involved in the national NHSE/I body worn camera’s pilot. The pilot is scheduled to span over 3-years and in due course an in-depth evaluation will take place as to the success of the pilot. NWAS also plan to undertake a local evaluation to understand learning. The phase 1 go-live date for 27 stations was set for the end of March 2021 and 21 stations achieved this date. Due to external IT delays the remaining 6 stations went live mid-April 2021. The phase 2 and 3 go-live date was set for May 2021; only 15 out of the 31 stations achieved this date. This was due to delays experienced with hardware delivery due to Covid-19 and again delays with external IT installations. By August 2021 all cameras were operational. Body worn cameras are now being embedded as business as usual and ongoing work is being undertaken to review camera uptake, IT elements, violence and aggression review against the project benefits and to identify any issues. To date this project has supported prosecutions.
Control of substances hazardous to health (COSHH)
During 2021/22 improvements were made to better control the process of approving substances used within NWAS that are subject to COSHH. The clarity of process now enables a product to be approved as safe for use within 24 hours.
Regulatory reform (Fire safety) order 2005 assurance (FSA)
In the annual report of 2020/21, it was recorded the impact of the pandemic upon the ability to undertake all the planned Fire safety risk assessments (FSAs). The HSS team developed FSA criteria which found according to risk the frequency an assessment should take place.
As a result, in 2021/22 58 FSA were required to be completed before 31 March 2022. This was achieved in full.
7.7.5. Infection, Prevention and Control (IPC)
Infection, prevention and control (IPC) practices are central to protecting the health, safety and welfare of patients, service users and staff, particularly in a global pandemic. Throughout the pandemic guidance has been updated on a regular basis to minimise the transmission of Covid-19 guidance is updated in line with national guidance on new variants and how to restrict further onward transmission during waves of the pandemic. In the last 12 months there has been drastic changes in the government advice on testing, isolation and vaccination of both the public and health care staff. Throughout the pandemic both clinical and operational bulletins have been issued by the IPC Team to clarify new guidance which were then cascaded through the operational command cells.
During 2021/22, the trust reviewed and updated the IPC board assurance framework focussing attention of the following 10 key lines of enquiry.
| IPC Board Assurance Framework Questions |
| Systems are in place to manage and monitor the prevention and control of infection. These systems use risk assessments and consider the susceptibility of service usersand any risks posed by their environment and other service users |
| Provide and maintain a clean and appropriate environment in managed premises that facilitates the prevention and control of infections |
| Ensure appropriate antimicrobial use to optimise patient outcomes and to reduce the risk of adverse events and antimicrobial resistance |
| Provide suitable accurate information on infections to service users, their visitors and any person concerned with providing further support or nursing/medical care in atimely fashion |
| Ensure prompt identification of people who have or are at risk of developing aninfection so that they receive timely and appropriate treatment to reduce the risk of transmitting infection to other people |
| Systems to ensure that all care workers (including contractors and volunteers) are aware of and discharge their responsibilities in the process of preventing andcontrolling infection |
| Provide or secure adequate isolation facilities |
| Secure adequate access to laboratory support as appropriate |
| Have and adhere to policies designed for the individual’s care and provider organisations that will help prevent and control infections |
| Have a system in place to manage the occupational health needs and obligations of staff in relation to infection |
Systems to manage and monitor infection and risks of infection
IPC guidance has been regularly updated throughout 2021/22 to ensure NWAS guidance is in line with national emerging guidance, particularly related to the management of nosocomial infection, testing and isolation, NWAS test, track and trace, outbreak management and working safely. Covid-19 risk assessments have been reviewed and updated as necessary. Service line assurance reports and results of IPC / hand hygiene / environmental audits are presented at the IPC subcommittee.
Provide and maintain a clean environment
Additional cleaning facilities and an increase in cleaning hours continued throughout 2021/22 based on footfall, layouts and occupancy and to support outbreak management. Enhanced cleaning of vehicles across hospital sites upon patient handover at emergency departments continued. Safety check points were maintained at all sites which included alcohol gel, face masks and thermometers. IPC audits continued and incorporated daily checks, weekly audits completed by operational managers and audits completed by IPC practitioners in line with the IPC audit tool enhanced with specific Covid-19 related questions. A ventilation assurance report was completed for both the trusts premises and the fleet of vehicles. Personal Protective Equipment (PPE) storage facilities were also reviewed. The evaluation of changes made to our outsources cleaning services during Covid-19 provided significant increased insight of the impact of outsourced cleaning on levels of cleanliness, time saved and staff satisfaction.
Ensure appropriate antimicrobial use to optimise patient outcomes and to reduce the risk of adverse events and antimicrobial resistance
Although clinical staff in the organisation do not prescribe or administer large numbers of antimicrobials, mandatory reporting requirements are completed, and assurance is presented to the Clinical Effectiveness sub-committee. Clinicians follow the Paramedic Drug Formulary for Antibiotics and JRCALC Guidance for Benzylpenicillin.
Provide suitable information on infections for staff and patients
Action cards were developed for crews managing infectious patients within vehicles and to support ventilation within vehicles. National guidance and local operating processes disseminated regularly to staff via bulletins, social media, internal intranet and the IPC cell. All training materials for staff and volunteers was reviewed. A routine data reporting system for outbreak data was designed and established utilising test, track and trace information to support outbreak management across sites.
Identification of people at risk of developing an infection and onward transmission Asymptomatic testing of trust staff continued throughout the year either by LAMP testing or the utilisation of lateral flow tests (LFT). Guidance on testing and self-isolation changed several times over the period and was often different to guidance for the public which increased confusion. A flowchart was developed to support decision making.
In January 2021, as a response to a national increase in Covid-19 cases due to the Omicron variant NWAS hosted a LAMP testing site for NWAS staff and their families at Broughton, the site was operational for a week and allowed staff to attend and receive a Covid-19 result within 6 hours of testing.
The NWAS test, track and trace service continued to provide the function of supporting staff members that tested positive for Covid-19 and to identify any staff or patients who may have been close contacts of the NWAS staff member. This service has been operational seven days a week over the year and at times during peak incidence has seen unprecedented demand leading to some delays in contacting staff and requiring staff to be pulled into the team to support. 3,856 staff members have had confirmed Covid-19 positive test results since we started recording this data in a secure and confidential way. 2311 staff were identified as close contacts of those staff members by the test, track and trace team.
Prevention of onward transmission was the main focus by ensuring that Infection control measures were being adhered to – these measures included: protective screens and barriers across call centres, reduced occupancy of offices and home working where appropriate, ventilation reviews across buildings and fleet, individual and environmental risk assessments, social distancing within PTS vehicles and mask/hood wearing. These control measures were implemented in partnership with trade union colleagues and in line with national Working Safely guidance.
Systems to ensure staff discharge their responsibilities for IPC
Weekly bulletins and guidance were regularly published for staff and available on the intranet.
All IPC policies are available to NWAS staff on the Green Room, IPC training packages and posters were updated and available for use by all staff. Short educational donning and doffing PPE and lateral flow test procedure videos for staff have been developed and distributed.
Fit testing policies were updated, and respiratory protective equipment hoods were fully rolled out across the organisation via a respiratory protective equipment steering group. Compliance with the use of hoods and level 3 PPE protection was measured with a bespokeaudit, which identified high compliance rates of 94% any challenges related to full compliance with PPE in particular circumstances, such as rapid patient deterioration and with babies and children. Learning and enquiry approaches have been taken to support staff to protect themselves and to discharge their responsibilities in these circumstances has been put into place.
Isolation facilities
Hospital handover action cards were developed 2020/21 and have continued to be used in line with national guidance for patients delayed during handover on the back of a vehicle. The cards supported staff to protect themselves and their patient whilst confined and isolated within the vehicle.
Access to laboratory support
Symptomatic health care staff have had priority access to PCR testing for Covid-19, there have been some delays in staff being able to obtain a test during periods of significant increase in Covid-19 cases in the community. Some local acute trusts have supported with PCR testing for NWAS staff during these periods.
Policies and training to prevent and control infections
National guidance was updated regularly in the last 12 months. Policies have been revised to reflect any changes and bulletins have been distributed to cascade information to all staff. The list below includes some of the guidance that has been amended but is not an exhaustive list:
- Working safely procedures including introduction of social distancing at work, masks, and screens
- Outbreak management procedures
- Test, track and trace procedures including adaption to sickness/absence reporting
- Lateral flow testing and reporting procedures
- Fit testing procedures
- Aerosol generating procedure audits
- Covid-19 Risk assessment
- Routine ventilation checks of vehicles via SafeCheck
- Introduction of local and strategic outbreak control meetings
- Enhanced audit of high-risk areas (high footfall) e.g. call centres
- Enhanced training for IPC practitioner team
- RRV car sharing Risk Assessment
Occupational health needs and obligations
All staff have had individual Covid-19 risk assessments and referred for occupational health advice and guidance as necessary. Alternative duties have been put in place as required. All staff have been encouraged to have the Covid-19 vaccinations and vulnerable staff were prioritised for vaccination provisions.
7.7.6. Medicines Management
A range of general medicines and controlled drugs (CDs) are stocked and administered to patients across NWAS. The medicines optimisation strategy (as a key element of the Right Care (Quality) strategy) provides the workplan for the medicines team and progress has been made against the medicines management pledges. The medicines management pledges are:
- Innovation and digital integration of medicines end to end processes.
- Patient Group Directions (PGDs) will be in place where needed with a robust governance framework.
- Support clinical effectiveness of medicines and staff training and development
- Systems and governance of the safe and secure handling of medicines (SSHM) will be reviewed and enhanced including whether NWAS should store and supply controlled drugs under licence.
- Systems for handling medicine related incidents will be improved.
Innovation and digital integration - During 2021/22 the use of an in-house vehicle check system called SafeCheck was further embedded into daily use across the trust since its launch in the previous year. Medicine stocks are documented into the system creating a digital vehicle medicines stock inventory. This allows expiry dates to be flagged for pro-active monitoring. Assurances can be given that vehicles have the minimum quantities of medicines available at the start of a shift and improves the tracking of medicines from station to vehicle.
- Controlled drug vehicle audits were reviewed and launched via SafeCheck to provide compliance reports for providing local and trust level assurance on the way vehicles manage their controlled drug stocks. Manager dashboards were created for localised monitoring and reports developed for sharing to identify improvement actions required and to demonstrate areas of good practice to be shared between sectors.
PGDs - All PGDs required are in place and in date. This year a new medicine with associated PGD has been approved for implementation in 2022/23. In addition, a clinical review of the use of midazolam and ketamine was undertaken, new PGDs produced, approved, staff trained and PGD implemented. We have excellent assurance on our sign off of PGDs within NWAS and positive feedback on the training programme. A new PGD policy was developed, approved and implemented providing a robust governance framework alongside the set up of the PGD Subgroup. A review of the handling of the Covid-19 vaccine was completed and provided excellent assurance on the safe and effective handling of the vaccine.
Clinical Effectiveness and Training - Co-amoxiclav, an antibiotic, has been approved for use in the management of open fractures in line with NICE guidance. An e-learning module has been developed and will be implemented in 2022 when the new medicine is launched.
- Following an audit of nerve agent counter measures antidotes one of the recommendations was to review the training. This has been done in conjunction with the NWAS CBRN Manager. This new e-learning module is complete and will be launched in 2022.
- An audit of the use of ondansetron, an anti-sickness medicine introduced in December 2018, has been conducted with good assurance of compliance with use in line with JRCACL guidance.
- An audit of the use of paracetamol intravenous infusion, also introduced December 2018, has been conducted. This showed it was being used for a wide range of indications but no use in children. It was approved to swap the strength kept from 500mg to 1g, this will be launched in 2022.
- Introduction of using naloxone intranasally. This is a new medicine for EMTs to use and a new route. This is a new route for paramedics. A training package has been developed and this will be launched in 2022.
Ketamine and midazolam review of use in clinical practice was the main focus in 2021/22.
This led to a full literature review of the evidence for use in specific clinical indications and a full review of the governance associated with the use of the medicines. These two medicines are classed as enhanced medicines and fall under the remit of the NWAS ‘Procedure for review of enhanced care interventions’. This led to the following changes:
- Updated PGDs for midazolam, flumazenil and ketamine with full review of doses, indications and staff permitted to use them
- Updated training with development of two e-learning modules and a face-to-face session.
- Development of an ‘Enhanced Drugs Checklist’
- Update of the Senior Clinical Intervention Log
- Set up of a central register for ketamine and midazolam
The PGDs went live and 98% and 97% of staff had completed the training for ketamine and midazolam respectively.
Safe and secure handling of medicines
NWAS has successfully gained a controlled drugs Home Office licence and has fully implemented the procurement, supply and distribution of controlled drugs in house mitigating the risk of relying on third party providers. A report monitoring controlled drug usage has been developed and is supporting our governance framework in providing assurance in the handling of controlled drugs alongside the controlled drugs audits for vehicles (updated this year) and ambulance stations.
Medicine related incidents
Areas of focus have been:
- Working with Quality Control Northwest and the Medicines and Healthcare
- Learning lessons bulletin published
- Improved security of controlled drugs at ambulance stations
- Improving the management of injectable medicines providing syringe labels, filter needles and syringe caps and individual medicine risk assessments
- Use of the new electronic patient record to resolve incidents
- Issued a bulletin about medical gases to support correct handling
- Working with other groups to withdraw the use of warming cabinets
- Reviewing the layout of NWAS material in the JRCACL app to minimise risk of errors
- Set up of a national Ambulance Sector Medicines Safety Officers Group has been set up within the AACE governance structure, chaired by NWAS Chief Pharmacist.
- Working with Quality Control Northwest and the Medicines and Healthcare roducts Regulatory Agency regarding faulty batches of amiodarone injection.
Serious incidents continue to be discussed at the Medicines Optimisation Group with recommendations made and actions overseen.
7.8. Care Quality Commission
As of 31st March 2022, the trust’s overall CQC ratings remain the same as the 2020/2021 Quality Account:
| Ratings | |
| NWAS overall rating | Good |
| Are services safe? | Good |
| Are services effective? | Good |
| Are services caring? | Good |
| Are services responsive? | Good |
| Are services well-led? | Good |
The trust’s overall CQC Inspection ratings matrix is as follows:
| Safe | Effective | Caring | Responsive | Well-led | Overall | |
| U&EC | Good | Good | Good | Outstanding | Good | Good |
| PTS | Good | Good | Good | Good | Requires Improvement | Good |
| EOC | Good | Good | Good | Good | Good | Good |
| Resilience | Good | Good | Not rated | Good | Good | Good |
| NHS 111 | Good | Good | Good | Good | Good | Good |
| Overall | Good | Good | Good | Good | Good | Good |
In 2021/2022 the CQC continued to regulate providers using a risk-based model under their transitional regulatory approach (TRA). This includes regular local level provider engagement meetings and a periodic transitional monitoring approach (TMA), via a multi- disciplinary documentation return and follow-up, virtual interview.
In January 2022, following the departure of the NWAS nominated individual (individual responsible for supervising the management of the regulated activity provided) due to retirement, submission for a new nominated individual was made and a revised Certificate of Registration was received.
In February 2022 the CQC announced a system level focussed inspection of the Lancashire and South Cumbria Integrated Care System (ICS) and each of the partner agencies within the ICS, which was following by an announcement of a similar inspection in North Mersey. CQC inspected Lancashire and South Cumbria and Merseyside areas; and NWAS during February-April 2022. NWAS and system partners are waiting for the outcome of the inspection.
7.9. Quality Assurance Visits (QAV)
NWAS has conducted annual Quality Assurance Visits (QAV) across PES, PTS and 111 service lines since 2012. The purpose of QAVs is to provide assurance to the trust about the quality and safety of our operational premises, vehicles, and services at sector level. QAVs include several health and safety focussed assessments in parallel to other audits such as the Health and Safety (HSS) snapshot audit and the Covid-19 risk assessment.
This internal rating system enables benchmarking and the recognition of outstanding areas of practice that can be celebrated and shared, ensuring as a trust we continue our journey towards achieving and maintaining excellence.
The purpose of Quality Assurance Visit (QAV) is to provide assurance to the trust about the quality and safety of our operational premises, vehicles, and services at sector level. After the QAV takes place, the nominated QAV lead produces a report comprising a summary of the key findings and an action log, which is then submitted to the Head of Service for sign off.
- A central repository of all QAV reports and actions is held on the trust’s knowledge management system, SharePoint. The overall position for QAV compliance across the trust (as at 01/04/2022) is outstanding with 100% of all operational sites having received a QAV in the last 12 months, despite Covid-19 operational pressures.
- Each sector has their own Integrated Action Tracker (IAT) which is stored on an Excel spreadsheet, which is centrally located in the trust’s knowledge management system, SharePoint. The IATs are managed locally by area administrators and contain actions from various audits (e.g., QAVs, Covid-19 risk assessments and HSS snapshot audits). As at the 1 April 2022, the current action completion position was strong with each area averaging at over 85% compliance for closure of QAV, HSS and Covid-19 risk assessment actions.
In 2020 NWAS commenced a collaborative internal programme of modernising the Quality Assurance Visit (QAV) process with a vision of aligning QAVs to the Care Quality Commission (CQC) inspection process, primarily through alignment to the CQC Key Lines of Enquiry (KLOEs) and the development of an internal rating system. This work has continued in 2021/22. This has ensured that the NWAS QAV internal framework is aligned to the five CQC KLOEs that apply to every health and social care setting: safe, effective, caring, responsive and well led.
To support the introduction of the new QAV process we have updated the QAV section on the trust intranet which hosts a newly developed suite of documents, an E-Learning module which is hosted on ESR for all staff who are involved or interested in the QAV process. This module supports a more consistent and informed approach to the QAV process.
7.10. Skills training
Due to the ongoing pressures around Covid-19, many training offers including mandatory training were paused again this year and reassessed based on training need analysis where appropriate, to ensure staff could focus on delivering patient care. The focus for 2021/22 has been to:
- Ensure the use of equality impact assessments to support decision making.
- Continue to progress safety culture and organisational culture via refreshed values and ‘Treat Me Right’ campaign.
- Establish systems for the measurement, monitoring and reduction of inequalities within programmes and across service lines where possible.
- Ensure recruitment, training and development opportunities are fair, open and transparent and open to all.
7.11. Equality Diversity and Inclusion
Promoting and supporting diversity in the workplace contributes towards employee wellbeing and engagement and a diverse workforce can drive an organisation’s effectiveness through enabling people to reach their full potential, in turn improving innovation and decision-making, as well as meeting the needs of a diverse population.
We continue to work with partners across the region and nationally in collaboration on activities and to share best practice about inclusion. We work proactively to be visible as an employer of choice across all our communities. We strive to reduce the health inequalities faced by our most vulnerable patients across the North West.
As we continue to recover and rebuild from the effects of the pandemic, we hope to emerge as an even more resilient, compassionate and considerate organisation for all our staff and patients, with a continued focus on seeing diversity and inclusion woven as golden threads through the fabric of organisational culture.
The trust is committed to creating a culture of openness and transparency. As a requirement of the Public Sector Equality Duty, the Trust must capture a range of equality related information and report on it and a statutory obligation under the Equality Act 2010 to publish a range of monitoring information relating to workforce, patients and the local community. This data and narrative includes the Workforce Race Equality Standard (WRES), Workforce Disability Equality Standard (WDES), Equality Delivery System (EDS), Gender Pay Gap Reporting and the Public Sector Equality Duties (PSED).
During 2021/22 a trust priority has been to embed equality, diversity and inclusions (EDI) across NWAS services and work programmes. Work to date includes:
- Continuing focus to integrate equality, diversity, and inclusion into all aspects of the Right Care strategy; working with NWAS staff networks (LGBT+, Race Equality, Disability, Armed Forces) to encourage involvement in quality programmes of work and to strengthen visibility, advocacy and intersectionality.
- Established systems for the measurement, monitoring and reduction of inequalities within programmes and across quality service lines using NHS staff survey, WRES, WDES, gender pay gap reporting to sustain and maintain representation.
- Ensuring recruitment, training and development opportunities are fair, open and transparent to all, supported by diverse panel members i.e., gender split and working with the NWAS Learning and Organisational Development manager with a focus on EDI.
- Ensuring the use of equality impact assessments to support decision making from the start of any work/project and taking views from wider stakeholders.
7.12. Right Care Strategy refresh
During 2021/22 engagement sessions have been held with various public and staff forums to understand what should be included in the refreshed Right Care strategy. These groups include PES, PTS, 111, Board, Patient and Public Panel, Race Equality Network, Disability Network, Senior Leadership Group. Staff feedback campaigns were also run via the staff intranet. The refresh of the trust and quality strategy are being run in parallel and will be available in summer 2022.
8. Looking Forward to Improving Care
8.1. 2022/23 Priority areas for improvement
Safety
- Continue to deliver actions out for the national patient safety strategy
- Triangulate data to enable the measurement and monitoring of safety as described in the measurement and monitoring of safety framework including real time and predictive measures
- Evaluate the impact of body worn cameras on violence and aggression
Effectiveness
- Two deep dives of safeguarding performance are completed in year
- Roll out digital clinical audit too
- All nationally mandated clinical data collections for the 999 service (“clinical audit”) are completed on time in full each month
- Continue our focus on ACQIs improvement
- Create the conditions for innovation, improvement and learning to improve wellbeing, quality, productivity, and efficiency
- Improve decision making through access to shared care records and onward referral pathways
- Enable access to mental health specialist support ensuring patients get the right care
- Deliver the learning disabilities and autism plan
Patient Centred - Embed patient and public engagement into the delivery of the Right Care strategy objectives
- Continue to develop the patient and public panel
Quality compliance - Ensure the trust maintains a ‘Good’ CQC rating
- Ensure the trust can deliver safe systems of work for staff in line with Health and Safety Executive regulatory standards
- Implement a new work programme aligned to the refreshed Quality strategy
- Further embed quality assurance visits including peer review
- Refine quality compliance measurement and use to drive improvement
- Refine processes for quality checks and re develop SafeCheck –our quality management system
Equality, Diversity and Inclusion - Increase focus and integrate equality, diversity and inclusion into all aspects of the quality strategy; work with staff networks to encourage involvement in quality programmes of work and to strengthen visibility, and advocacy
- Incorporate EDI measures into the Integrated Performance Report
- Increase ethnicity data capture
- Increase access to translation services including British Sign Language
- Deliver the Mental health plan to ensure equity of response for Mental health Patients and implement the staff suicide prevention toolkit
- Develop a plan for digital inclusion
9. Formal Statements on Quality
9.1. Review of Services
The trust has reviewed all the data available on the quality of care in the services provided by us in 2021/22. The income generated by the NHS services reviewed in 2021/22 represents 100% of the total income generated from the provision of NHS services by the trust.
9.2. Participation in Clinical Audits
NHS England Ambulance Quality Outcome Indicators English ambulance services are required to undertake specific ambulance clinical audit and submit the data according to a prefixed schedule directly to NHS England.
The list of mandated audits is:
Outcome from cardiac arrest – return of spontaneous circulation (ROSC):
- Overall
- Utstein comparator group
Outcome from cardiac arrest – survival to discharge:
- Overall
- Utstein comparator group Post ROSC Care Bundle:
- The number of patients who received the appropriate care bundle after sustaining ROSC for 10 minutes or longer after an out-of-hospital cardiac arrest where resuscitation (advanced or basic life support) was commenced/continued by ambulance service.
Outcome from acute ST-elevation myocardial infarction (STEMI):
- Time from call to angiography
- The number of patients with a pre-hospital diagnosis of suspected ST elevation myocardial infarction confirmed on ECG who received the appropriate care bundle
Outcome from stroke:
- Time from call to hospital arrival
- The number of Face Arm Speech Test (FAST)- positive or suspected stroke patients assessed face-to-face who received the stroke diagnostic bundle
Outcome from sepsis:
- The number of patients with suspected sepsis with a NEWS of 7 or above assessed face-to-face who received an appropriate care bundle
It is anticipated that in 2022/23 the outcome from sepsis measure will be retired and replaced by a pilot measure reviewing the care received by patients who are over 65 years, have fallen from a standing height or less and discharged at scene. This patient cohort accounts for 10-25% of emergency ambulance responses each year. The rationale for the new audit is driven through falls association with increased morbidity and mortality, therefore having an impact on quality of life, health, and healthcare costs. It is important to assess the practice and behaviour that our ambulance clinicians provide to this patient cohort when discharging at scene.
9.3. Participation in Clinical Research
North West Ambulance Service (NWAS) NHS Trust is dedicated to providing high quality care to our patients by meeting not only their immediate healthcare needs, but also having a positive impact on their future health and wellbeing. As an NHS organisation, we have a responsibility to provide our patients, staff and the public with the opportunity to participate in health care research.
Our research strategy expresses our commitment to host and develop research that will not only enhance the quality of the urgent and emergency care we deliver but will ensure that the communities we serve have equitable access to our high quality, clinical services to continue improving the health outcomes for all of our patients.
Our mission is to embed a culture of research excellence and to be at the vanguard of generating new evidence that supports the delivery of first-rate, urgent, and emergency care.
Our vision is to enhance the health and wellbeing of the communities we serve by translating high quality research into exceptional service provision and outstanding clinical practice.
The medical directorate is accountable for research at the trust. Under the direction of our consultant paramedic in their capacity as research lead, we have continued to make strides in embedding research across our organisation.
We sustained income from the National Institute for Health and Care Research Clinical Research Network (NIHR CRN) to support a full-time, NIHR research paramedic who delivers and promotes NIHR research throughout the organisation. We expanded the Research & Development (R&D) team through the additional appointments of an NIHR grant funded research paramedic, an NIHR research practitioner and a research support officer.
For the second consecutive year, the trust successfully triggered NIHR Research Capability Funding (RCF) by recruiting at least 500 individuals to non-commercial research studies conducted through the NIHR CRN. The purpose of NIHR RCF is to help research-active NHS organisations to act flexibly and strategically to maintain research capacity and capability and to support the appointment, development and retention of key staff undertaking or supporting patient-based research.
We had our first Chief Investigator for our first NIHR industry clinical trial and our staff took on the roles of Principal Investigator and Local Collaborator for NIHR CRN Portfolio studies.
We continued to offer support for researcher development. A staff member was awarded a Data Science Internship by NIHR Applied Research Collaboration North West Coast and we offered a PhD studentship in collaboration with Lancaster University and Liverpool University.
We publicised research opportunities, successes, and achievements both internally and externally through regular communications bulletins, social media and via dedicated pages on both the trust internet and intranet. With the NWAS Staff App that allows for subscribers to be notified of new research studies that staff can be involved in delivering or participating in.
We actively maintained partnerships with our local NIHR Applied Research Collaborations (ARCS) and CRNs in Greater Manchester and North West Coast, through which we engage with health and care providers, academia and other external stakeholders to cultivate research collaborations.
We remained an active member of the National Ambulance Research Steering Group (NARSG) through which we access opportunities to be involved in grant applications and upcoming research studies, enhancing our reputation as a research-active organisation.
9.3.1. Performance in Clinical Research
During 2021/22, we opened 13 new research studies that were approved by a research ethics committee.
11 of the newly approved research studies were NIHR CRN Portfolio studies to which we successfully recruited 625 research participants including staff, patients and the public, figure 11 below.
| National Institute for Health Research Clinical Research Network Portfolio Performance | ||||
| Financial Year | 2018/19 | 2019/20 | 2020/21 | 2021/22 |
| Number of Studies Open to Recruitment | 4 | 7 | 6 | 11 |
| Participants in Studies | 65 | 645 | 606 | 625 |
The NIHR CRN Portfolio research studies we sanctioned in 2021/22 included:
- Should I stay or should I go? NHS staff retention in a post Covid-19 world, challenges and prospects.
- AHP perceptions of NHS research capability and culture: A national research capacity in context survey.
- Community First Responders’ role in the current and future rural health and care workforce.
- Prehospital feedback in the United Kingdom: A realist evaluation of current practice using a multiple-case study design.
- ASPIRE-COVID-19 CENTRE: Achieving Safe and Personalised maternity care in response to epidemics – Case studies of eight NHS Trusts in England.
- The Resilience Hubs: A multi-site, mixed-methods evaluation of an NHS Outreach,
Screening and Support Navigation service model to address the mental health needs of key workers affected by the Covid-19 pandemic.
- A qualitative study exploring the experiences of research paramedics working in the UK.
- CESSATION: A mixed-methods study of female ambulance staff experiences of the menopause transition.
- Optimising Implementation of Ischaemic Stroke Thrombectomy (OPTIMIST): exploring NHS professional views about the emergency stroke pathway. CI, Dr Jo Day, University of Exeter.
- Pre-hospitAl RAndomised trial of MEDICation route in out-of-hospital cardiac arrest (PARAMEDIC3). Prehospital feedback in the United Kingdom: A realist evaluation of current practice using a multiple-case study design.
- Prehospital feedback in the United Kingdom: A realist evaluation of current practice using a multiple-case study design.
In 2021-22, the trust issued research management approval for 2 non-Portfolio studies:
- Exploring the impact of the Covid-19 pandemic on undergraduate student paramedic learning, confidence and readiness for clinical practice in a UK Ambulance Service.
- Enhancing Pre-hospital Chest Pain Telephone-triage using a Prediction Model
9.3.2. Research Grants
NWAS was a co-applicant for a successful bid for the Movember and The Distinguished Gentleman’s Ride Veterans and First Responders Mental Health Grant Program, a collaboration led by the University of York. The Behavioural Activation for Low Mood and Anxiety in Male NHS Frontline Workers (BALM) research programme aims to develop, deliver and evaluate a gender-sensitised Behavioural Activation (BA) programme to help improve common mental health challenges such as low mood, burn-out, anxiety and depression faced by male NHS staff.
9.3.3. Research Publications
The following research publications were either authored or co-authored by staff at North West Ambulance Service NHS Trust in the financial year 2021/22 and are listed in the Ambulance Research Repository (AMBER) which is maintained by the Library and Knowledge Service for NHS Ambulance Services in England:
- Alotaibi, A., Body, R., Carley, S. and Pennington, E. (2021). Towards Enhanced Telephone Triage for Chest Pain: a Delphi Study to Define Life- Threatening Conditions That Must Be Identified. BMC emergency medicine [online], 21 (1), pp.158-158. DOI:10.1186/s12873-021-00553-w
- Alqurashi, N., Alotaibi, A., Bell, S., Lecky, F. and Body, R. (2022). The diagnostic accuracy of prehospital triage tools in identifying patients with traumatic brain injury: A systematic review. Injury: International Journal of the Care of the Injured [online]. DOI: 10.1016/j.injury.2022.02.020
- Bell, S., Pennington, E., Hill, J. and Harrison, J. (2022). Prehospital airway management. Journal of Paramedic Practice: the Clinical Monthly for Emergency Care Professionals [online], 14(2), pp.51–53. DOI: 10.12968/jpar.2022.14.2.51
- Hetherington, J. and Jones, I. (2021). What factors influence clinical decision making for paramedics when attending to paediatric emergencies in the community within one ambulance service trust? (2021). British Paramedic Journal [online], 6(1), pp.15-22. DOI: 10.29045/14784726.2021.6.6.1.15
- Holland, M., Dutton, M. and Glover, S. (2021). How it’s done: search tools and techniques for major bibliographic databases. Journal of Paramedic Practice : the Clinical Monthly for Emergency Care Professionals [online], 13(5), pp.210–
- 213. DOI 10.12968/jpar.2021.13.5.210
- McElroy, L., Robinson, L., Battle, C., Laidlaw, L., Teager, A., de Bernard, L., McGillivray, J., Tsang, K., Bell, S., Leech, C., Marsden, M., Carden, R., Challen, K., Peck, G., Hancorn, K., Davenport, R., Brohi, K. and Wilson, M. S.
- J. (2021). Use of a modified Delphi process to develop research priorities in major trauma. European Journal of Trauma and Emergency Surgery [online], pp.1–9. DOI: 10.1007/s00068-021-01722-z
- Rollinson TJ, Furnival J, Goldberg S, and Chowdury, A. (2021). Learning from Lean: a quality improvement project using a Lean-based improvement approach to improve discharge for patients with frailty in an acute care hospital BMJ Open Quality; 10:e001393. doi:10.1136/bmjoq-2021-001393
- Thomson, G., Balaam, M-C, Nowland Harris, R., Crossland, N., Moncrieff, G., Heys, S., Sarian, A., Cull, J., Topalidou, A. and Downe, S. (2022). Companionship for Women/birthing People Using Antenatal and Intrapartum Care in England During Covid-19: a Mixed-Methods Analysis of National and Organisational Responses and Perspectives. BMJ open [online], 12(1) pp.e051965-e051965. DOI:10.1136/bmjopen-2021-051965
9.4. Use of the CQUIN Payment Framework
The trust has not been involved in any Commissioning for Quality and Innovation (CQUIN) payment schemes during 2021/22 as the national NHS contracting process was halted due to Covid-19. During this recovery period there are national discussions underway relating to the future contracting and commissioning process which may impact on the CQUIN payment framework. The National Tariff payment system (NTPS) consultation document and NHS Standard Contract propose that CQUIN will be brought within the scope of the NTPS.
10. Statement on Relevance of Data Quality and Improvements
Please find the North West Ambulance Service NHS Trust statements on data quality;
- NHS Number and General Medical Practice Code Validity
North West Ambulance Service NHS Trust did not submit records during 2021/22 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. This requirement did not apply to ambulance trusts during 2021/22. - Clinical coding error rate
North West Ambulance Service NHS Trust was not subject to the Payment by Results clinical coding audit during 2021/22 by the Audit Commission. - Data Security and Protection Toolkit (DSPT) attainment levels
North West Ambulance Service NHS Trust DSPT baseline submission assessment provided an overall score for 2021/22 was 99.09% (109 of the 110 compliance standards were met) with a published status of ‘standards not met’.
After feedback from external auditors the assertion NWAS failed to meet compliance for the Data Security and Protection Toolkit was compliance with information governance training. The action being taken during 2022/23 is the NWAS Information Governance and Learning and Organisational Development team are proactively working together to look at a solution to increase mandatory training compliance.
11. Clinical Commissioning Groups, Healthwatch and Health Scrutiny Committee Statements
The trust works in collaboration with all partners and the Quality Account has been shared with external partners including Commissioners, Providers, Councils and Healthwatch groups. Comments received are noted below:
Lancashire County Council Health Scrutiny Committee
The Lancashire Health Scrutiny function welcomes the opportunity to comment on the North West Ambulance Service NHS Trust’s Quality Accounts for 2021/22.
The trust should be commended for the format and structure of the report especially given the range of information the trust is required to reference. In particular it was felt the feedback from public and staff was well set out.
It was felt further narrative could have been provided to help explain the sections on paramedic emergency services and the emergency operation centre. In addition, it was felt examples of patient experience would have helped to provide the reader with a personal touch. The trust should be commended for including a breakdown of those matters raised under the Freedom to Speak Up policy.
Overall, members were in favour of the production of a summary, or easy read document with the main content and findings of the Quality Account accessible to the public as the key audience.
It was felt the report was a fair reflection of the trust’s position and whilst members acknowledged the difficulties faced by the organisation in Lancashire, there remained some concerns around performance. The Lancashire health scrutiny function remains committed to finding ways to assist the trust and add value.
The Lancashire Health Scrutiny function would welcome early involvement with the planning process for the production of the trust’s 2022/23 Quality Account.
Oldham Council
It is evident that the North West Ambulance Service remains under considerable pressure and, as with many other public services, continues to be under resourced. The service is faced with increased demand and is being asked to “do more with less”. There can only be so many efficiencies that can be identified and achieved. For these to succeed, it has to be assumed that all other stakeholder are able to achieve similar results.
The wider community continues to be full of admiration for the paramedics who attend in response to each emergency. They continue to maintain a professional approach in every situation that arises and is a tribute to their resilience that they continue to cope despite mounting pressures.
The NHS continues to undergo change. In Greater Manchester, the integrated care service comes into being in a few weeks. All aspects of the NHS need to be able to work together with local authorities and other public bodies to ensure it continues to serve the wider community and the benefits of continuing cooperation become apparent.
I hope that this statement is of some value. Colin McLaren
Councillor
Chadderton Central Ward
Healthwatch Cumbria
- Statement on quality from the Chief Executive
A concise introduction giving examples of key achievements during 2021-22. The CEO also pays tribute to the contribution made by all staff during a time of unprecedented pressure on NHS services.
- Trust Overview
This section contains a helpful summary of the framework which will operate with multiple ISC NHS bodies and the governance arrangements.
- Trust Vision and Aims
We note the creation on the Right Care strategy and welcome the inclusion of the public through engagement work to contribute to future trust and quality strategies.
- Services
From the list of services delivered we would compliment the Trust for creating and maintaining the largest and longest established Community First Responder (CFR) schemes in England to provide support within communities, likewise for the support to volunteer drivers and the volunteers contributing to the Patient and Public Panel.
- Operational Performance
This contains some very useful data regarding response times, the challenges faced and remedial actions. We were pleased to see the Trusts achievement in compliance with core standards with the EPRR arrangements and despite pandemic restrictions the work done to deliver a safe and effective service.
Sections 5 – 8
A comprehensive description of areas of focus during 2021-22. We would highlight the following:
- We liked the linking of digital systems, access to British Sign Language interpreters on scene, safety skills training, employment of s full-time patient safety specialist, appointment of a new consultant midwife, the work done regarding mental health support.
- We thought that the Freedom to Speak Up report was very comprehensive and pleased to see the positive developments to create a healthy speaking up culture.
- The work done regarding handover delays and the implementation of the ‘Ambulance Handover Delays Managers Escalation action card’.
- The Right Care at Home aimed at reducing hospital admissions by Ambulance utilising triage tools to support patient care.
- We liked the patient and public engagement, particularly recruitment of young people and the themes identified for further improvement.
9. Formal Statements and Audits
We believe that NWAS has participated in all the required audits. Excellent Glossary of Terms.
Healthwatch Cumbria considers this to be a transparent, well presented, informative document, clear identification of areas to improve and actions taken. We look forward to seeing future collaboration with patients, families, staff and partnership working contributing to the delivery of tangible improvements.
Oliver Pearson Manager Healthwatch Cumbria
Appendix 1: Glossary of Terms
| ABBREVIATION | DESCRIPTION |
| 4AT | The 4 ‘A’s Test (4AT) is a bedside medical scale used to help determine if a person has positive signs for delirium. The 4AT alsoincludes cognitive test items, making it suitable also for use as a rapid test for cognitive impairment. |
| 6S | 6S is a quality improvement process tool that stands for sort, set in order, shine, standardise, sustain and safety. |
| AACE | The Association of Ambulance Chief Executives provides ambulance services with a central organisation that supports, coordinates, andimplements nationally agreed policy. |
| Advanced Paramedics | Advanced paramedics offer a high level of clinical skills and leadership. They co-ordinate and provide clinical advice for some of the more complex incidents we attend, whilst also being responsiblefor a team of senior paramedics. |
| AED | Automated external defibrillators |
| AGM | Annual general meeting is a yearly gathering between the NWAS board of directors, staff, patients and public to discuss performance,service delivery and strategic direction. |
| AMBER | Ambulance Research Repository. |
| ARP | Ambulance Response Programme: In 2017, following the largest clinical ambulance trials in the world, NHS England implemented new ambulance standards across the country. This was to ensure the sickest patients get the fastest response and that all patients get theright response first time. |
| BAF | Board assurance framework is used to record and report an organisational key strategic objectives, risks, controls and assurancesto the board. |
| C1 | Category 1: An immediate response to a life-threatening condition,such as cardiac or respiratory arrest. Response time to 90% of all incidents is 15 minutes. |
| C2 | Category 2: A serious condition, such as stroke or chest pain, which may require rapid assessment and/or urgent transport. Responsetime to 90% of all incidents is 40 minutes. |
| C3 | Category 3: An urgent problem, such as an uncomplicated diabeticissue, which requires treatment and transport to an acute setting. Response time to 90% of all incidents is 2 hours. |
| C4 | Category 4: A non-urgent problem, such as stable clinical cases, which requires transportation to a hospital ward or clinic. Response time to 90% of all incidents is 3 hours. |
| Cardiac arrest | A medical condition wherein the heart stops beating effectively, requiring CPR and sometimes requiring defibrillation. |
| CAS | A Clinical Assessment Service can operate within primary care or secondary care and be directly bookable or indirectly bookable. |
| CCG | Clinical Commissioning Groups (CCGs) were created following the Health and Social Care Act in 2012 and replaced Primary Care Trusts on 1 April 2013. They are clinically led statutory NHS bodies responsible for the planning and commissioning of health careservices for their local area. |
| CEO | Chief Executive Officer. |
| CHUB | The Clinical Hub is a department within the NWAS emergencyoperations centres that is made up of a multidisciplinary team including clinicians, dispatchers, navigators and managers. |
| Cleric | Ambulance software solution. |
| Community First Responder (CFR) | A member of the public who volunteers to provide an immediate response and first aid to patients requesting ambulance assistance. |
| Complementary Resources | Non ambulance trust providers of potentially life-saving care, e.g.CFRs St John Ambulance, Red Cross, Mountain Rescue, Air Ambulance. |
| CCA | Civil Contingencies Act, 2004 requires NHS organisations, and providers of NHS-funded care, to show that they can deal with a wide range of incidents and emergencies that could affect health or patientcare while maintaining services. |
| CPR | Cardiopulmonary Resuscitation. |
| CQC | Care Quality Commission is the independent regulator of all health and social care services in England. |
| CQUIN | The Commissioning for Quality and Innovation (CQUIN) framework supports improvements in the quality of services and the creation ofnew, improved patterns of care. |
| Datix Cloud IQ | Datix Cloud IQ is a profound shift in focus for a healthcare risk management application, moving beyond the simple capture andreview of data on adverse outcomes towards a managed process of exposing and resolving the issues that lead to those outcomes. |
| Defibrillator (also AED) | Medical equipment to provide an electric shock to a patient’s heart which is not functioning properly. |
| DoS | The Directory of Services (DoS) is a central directory that is integrated with NHS Pathways and is automatically accessed if the patient does not require an ambulance or by any attending clinician in the urgentand emergency care services. |
| DSP | The Data Security and Protection Toolkit is an online self-assessment tool that allows organisations to measure their performance against the National Data Guardian’s 10 data security standards. All organisations that have access to NHS patient data and systems must use this toolkit to provide assurance that they are practising good datasecurity and that personal information is handled correctly. |
| Duty of Candour | Every health and care professional must be open and honest with patients and people in their care when something that goes wrong with their treatment or care causes, or has the potential to cause,harm or distress. |
| EOC | Emergency Operational Control receives and responds to 999 calls and other calls for ambulance service assistance. |
| EPR | Electronic Patient Record is a periodic health care record of a single individual, provided mainly by one healthcare organisation. |
| ERISS | ERISS is a web-based application, designed to enhance information sharing and collaborative working between the North West Ambulance Service (NWAS) and its key stakeholders. The system supports the transfer of referral information to external organisations in the North West and provides a secure portal for organisations to inform NWAS of care planning arrangements for specific patientgroups. |
| EPRR | Emergency Preparedness, Resilience and Response is an NHSorganisational plan for, and response to, a wide range of incidents and emergencies that could affect health or patient care. These could |
| be anything from extreme weather conditions to an outbreak of an infectious disease or a major transport accident. | |
| EMM | Every Minute Matters is a NWAS collaborative handover quality improvement programme. |
| ETA | Estimated time of arrival for an ambulance. |
| FAST | A simple test for the presence of a stroke – Face, Arms, Speech, Time. |
| FFT | The NHS Friends and Family Test was created to help service providers and commissioners understand whether patients are happy with the service provided, or where improvements are needed. It is a quick and anonymous way to give your views after receiving NHS careor treatment. |
| FTSU | Freedom to speak up. |
| Green room | Internal digital communication area for NWAS staff. |
| HSE | Health & Safety Executive is a regulatory body to ensure safe working practices are adhered to. |
| ICS | Integrated care systems (ICSs) are new partnerships between the organisations that meet health and care needs across an area, to coordinate services and to plan in a way that improves population health and reduces inequalities between different groups.Integrated Care Systems Design Framework, June 2021 Report template – NHSI website (england.nhs.uk) |
| Integrated Care Board | Each Integrated Care System (ICS) will have an Integrated Care Board (ICB), a statutory organisation bringing the NHS together locally to improve population health and establish shared strategic priorities within the NHS. When ICBs are legally established, clinicalcommissioning groups (CCGs) will be abolished. |
| IPC | Infection Prevention and Control. |
| KLOE | Key line of enquiry is part of the CQC’s inspection structure, which help establish whether services are Safe, Caring, Responsive,Effective and Well-led. |
| Just Culture | Just Culture is about creating a culture of fairness, openness and learning in the NHS. This is to make colleagues feel confident to speak up when things go wrong, rather than fearing blame. Supporting colleagues to be open about mistakes allows valuablelessons to be learnt. |
| LAMP testing | Loop-mediated isothermal amplification (LAMP) testing is a saliva testused to detect Covid-19 infections. LAMP testing is comparatively more efficient and cost-effective than PCR testing. |
| Language Line | A UK language translation service agency that provides a wide range of interpreting, translation and localisation agency services. |
| Lateral flow testing | A lateral flow test is a Covid-19 test you do yourself. It shows you the result on a handheld device that comes with the test. |
| MACA | Requests for Military Aid to the Civil Authorities (MACA) from the NHS in England |
| MBRRACE | MBRRACE-UK: Saving Lives, Improving Mothers’ Care report covers the lessons learned to inform care from rapid reviews of the care of women who died with SARS-CoV-2 infection or from mental health-related causes or domestic violence between March and May 2020. |
| NACQI/ACQI/AQI | National Ambulance Clinical Quality Indicator. |
| NHSE/I | NHS Improvement and NHS England have worked together as asingle organisation since 1 April 2019, to help improve care for patients and provide leadership and support to the wider NHS. |
| NHS Pathways | NHS Pathways is a clinical tool used for assessing, triaging and directing the public to urgent and emergency care services. |
| NIHR Applied Research Collaborations | The National Institute for Health Research (NIHR) is the nation’s largest funder of health and care research and provides the people, facilities and technology that enables research to thrive. NIHR Applied Research Collaborations (ARCs) support applied health andcare research that responds to, and meets, the needs of local populations and local health and care systems. |
| NIHR CRN | National Institute for Health Research Clinical Research Network. |
| NQB | National Quality Board. |
| NRLS | National Reporting and Learning System. |
| NTPS | National Tariff payment system is a set of prices and rules to helpcommissioners and providers of NHS care provide best value to their patients. |
| NWAS | North West Ambulance Service NHS Trust. |
| Ockenden report | The Ockenden report found a string of “repeated failures” spanning a period of 20 years – including at least 304 cases where there was avoidable harm. As a result of these failures, babies died or were leftseriously disabled owing to catastrophic mistakes at the Shrewsbury and Telford Hospital NHS Trust. |
| OPTIMIST | OPTimising IMplementation of Ischaemic Stroke Thrombectomy |
| Patient Safety IncidentReporting Framework | Patient Safety Incident Response Framework (PSIRF), outlines how providers should respond to patient safety incidents and how and when a patient safety investigation should be conducted. |
| Paramedic | A state registered ambulance healthcare professional. |
| PCN | Primary care networks are groups of practices working together to focus local patient care. |
| PDSA cycles | The Plan-Do-Study-Act cycle is shorthand for testing a change i.e. by planning it, trying it, observing the results, and acting on what is learned. This is the scientific method, used for action-orientedlearning. |
| PES | Paramedic Emergency Service responds to 999 emergency ambulance calls. |
| PHSO | Parliamentary and Health Service Ombudsman investigatecomplaints independently and impartially about government departments and the NHS in England. |
| Power BI | Power BI is a collection of software services, apps, and connectors that work together to turn your unrelated sources of data intocoherent, visually immersive, and interactive insights. |
| PPCI | Primary Percutaneous Coronary Intervention – treatment of a MI through immediate surgical intervention. |
| PPE | Personal protective equipment protects the user against health or safety risks at work. |
| PPP | Trust’s Patient and Public Panel consists of volunteers who live in the North West of England and are involved in public and patient engagement activities e.g. Responding to surveys, giving feedbackon publications, focus groups activities, attending committees or formal meetings. |
| PSI | Patient safety incidents. |
| PTS | Patient Transport Service – Non-emergency transport service that provides for hospital transfers, discharges and outpatients appointments for those patients unable to make their own travelarrangements. |
| Q&S | Quality and Safety Group meeting which is part of NWAS’s governance structure. |
| QI | The term ‘quality improvement’ refers to the systematic use of methods and tools to try to continuously improve quality of care and outcomes for patients. There are a range of different methods and tools, such as Lean, Six Sigma and the Institute for HealthcareImprovement’s Model for Improvement. |
| Quality Surveillance Group | The aim of a Quality Surveillance Group (QSG) is to identify risks to quality at as early a stage as possible. The group should ensure that action is taken to mitigate these risks, resolve issues locally where possible and drive improvement in quality in an aligned and coordinated way. These groups feed into the regional Quality Surveillance Group. NWAS and Commissioners are invited to all ICSQSG’s in line with national guidance. |
| RCF | Research capability funding. |
| RCQAC | Regional Clinical Quality Assurance Committee. |
| RIDDOR | Reporting of Injuries, Diseases and Dangerous Occurrences Regulations |
| ROSC | Return of Spontaneous Circulation. |
| ROSE | Review of serious events (ROSE) group oversees the reporting, actions and learning drawn from serious incidents. |
| SafeCheck | SafeCheck is an electronic database which was originally designed to replace paper process checks e.g. vehicle, equipment and medicinecheck book. SafeCheck is now being used captured routine audit work e.g. Infection Prevention and Control. |
| SDEC | Same day emergency care is one of the many ways the NHS is working to provide the right care, in the right place, at the right time forpatients. It aims to benefit both patients and the healthcare system by reducing waiting times and hospital admissions, where appropriate. |
| Service Finder | Service finder enables clinicians to review where appropriate alternative services are available to refer patients to when A&E is not suitable. The regional Directory of Service (DOS) lead has developedambulance referrals to ensure services most appropriate for NWAS clinicians are highlighted quickly. |
| SharePoint | SharePoint is a digital platform that enables document sharing and news updates. |
| SJR | Structured judgement reviews are a methodology used for investigations. |
| SMARTprogramme | NWAS’s internal digital and quality improvement programme. |
| SMS | Short messaging service- text messaging service component of most telephone, Internet, and mobile device systems. |
| Social prescribing | Social prescribing is a community referral which enables GPs, nurses, paramedics and other health and care professionals to refer peopleto a range of local, non-clinical services. |
| SPTLs | Senior paramedic team leader working as part of a crew or as a solo responder to attend urgent and critical emergency situations in avariety of environments. They use advanced clinical skills and manage a clinical team. |
| Standard Contract | The NHS Standard Contract is mandated by NHS England for use by commissioners for all contracts for healthcare services other thanprimary care. |
| StEIS | Strategic Executive Information System. |
| STEMI | ST Elevation Myocardial Infarction – A life threatening heart attack. |
| Stroke | Blockage or bleeding of the blood vessels in the brain that can lead to death or disability. |
| TMA | CQC are evolving their approach to regulation as the risks from Covid- 19 change. They are using a transitional monitoring approach toservices, which focuses on safety, how effectively a service is led and how easily people can access the service. |
| TRA | Transitional regulatory approach is a new CQC inspection way of working which has emerged during Covid-19. Inspectors will now review the information they hold about a service, and they will then either have a conversation with a provider online or by telephone. During the conversation, inspectors will ask providers ‘monitoring questions’ which will focus on specific KLOEs. |
| Utstein | Cardiac arrest and CPR outcome reporting process. |
Appendix 2: Contact Details
If you have any questions or concerns after reading this report please do not hesitate to contact the trust.
We can be contacted at:
North West Ambulance Service NHS Trust Trust Headquarters
Ladybridge Hall Chorley New Rd Bolton Lancashire
BL1 5DD
For general enquiries please use:
Telephone: 01204 498400
E-mail: [email protected]
For enquiries specific to the Quality Account, please contact Joy Furnival Chief of Regulatory Compliance and Improvement on:
Telephone: 01204 498400
E-mail: [email protected]
Should you wish to access any of the trust publications mentioned in this Quality Account they can be accessed on the trust website at www.nwas.nhs.uk.